Enhancing the immune system’s response to prostate cancer

Grant information
Reference: RIA23-ST2-007
Lead researchers:
Professor Ian Mills, University of Oxford
Associate Professor Harri Itkonen, University of Helsinki and University of Oslo
Award: £444,157
What you need to know
- This project explores a new way to treat prostate cancer by boosting the body's immune response to cancer cells.
- The researchers are testing drugs that could make prostate cancer cells more visible to the immune system, which could enable doctors to use immunotherapy to treat the disease.
- The aim is to gather enough evidence to start clinical trials, potentially leading to a new, more effective combination treatment for prostate cancer.
Why are we funding this research?
Prostate cancer is the most common cancer in men in the UK, causing around 12,000 deaths each year. Despite this, current treatments are not always effective, especially for aggressive forms of the disease, so new, more effective treatments are needed.
Unfortunately, one major challenge to developing new treatments is that the body's immune system doesn't always recognise and attack prostate cancer cells. This means that immunotherapy – which has been an extremely effective kind of treatment for other kinds of cancer – doesn't usually work in prostate cancer.
This research aims to change that by using drugs that make prostate cancer cells more visible to the immune system.
The initial discoveries paving the way for this work were made by Dr Itkonen when he was a PhD student in my group. It has been a privilege to be involved in this work through subsequent collaboration between his group and mine, and it is a pleasure to now jointly lead this project, which has the potential to change the way we treat prostate cancer.
What will the researchers do?
The researchers have found that blocking a protein called CDK9 can make prostate cancer cells more recognisable to the immune system. In this project, they will test drugs that block CDK9 to see how and if they work. These drugs have already been tested and found safe in other types of cancer.
To see if these drugs work, the researchers will first test them in mice. They will use two types of mice: regular mice and mice that have been modified to have a human-like immune system. This helps the researchers understand how the drugs might work in humans.
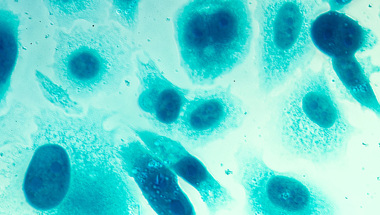
The researchers will also test the drugs on lab-grown mini-tumours called organoids. Unlike traditional lab models of cancer, where cells are studied flat in a dish, these 3D models are more reflective of real-life conditions – making them invaluable for testing new treatments. These organoids are grown from prostate cancer cells donated by men with the disease. When these cultures are combined with the immune cells from the same man, it is possible to assess if the drug enhances the immune cells’ ability to kill the tumour cells. This step is crucial because it shows how the drugs are likely to work on real human cancer cells.
Throughout these tests, the researchers will be looking at two main things: whether the drugs are safe and whether they effectively help the immune system attack the cancer cells. They need to make sure the drugs don't cause harmful side effects and that they actually improve the immune system’s response to prostate cancer.
If the tests in mice and organoids are successful, the next step would be to plan clinical trials where these drugs could be tested in people with the disease.
This work has developed from a project I began earlier in my career, and which has since been taken forward by two of my talented PhD trainees, Shivani Yalala and Aishwarya Gondane. The dedicated support from Prostate Cancer UK now enables us to further develop our discoveries. I am excited to have Professor Mills and the rest of our teams to potentially turn our initial discovery to a curative therapy against prostate cancer.
How will this benefit men?
By testing these drugs in both mice and prostate cancer samples from men, the researchers aim to gather enough evidence to start clinical trials. If these trials are successful, it could lead to a new treatment that helps the immune system fight prostate cancer more effectively, providing hope for men who currently have limited options. This could mean longer survival times, better quality of life, and fewer men dying from prostate cancer.
Help us fund more research like this
Your donation helps us fund lifesaving research into better treatments for prostate cancer.