Prostate cancer diagnosis in trans women
This page describes the steps to getting a diagnosis if you’re a trans woman, non-binary person assigned male at birth, or an intersex person who has a prostate.
We explain how you can get a prostate specific antigen (PSA) blood test and what your test results might mean. We also go through what to expect if you have a prostate examination, and what tests you might have at the hospital.
We know it can be difficult to talk about prostate problems if you’re a trans woman, non-binary or intersex, so we've created a checklist for talking to your GP about prostate cancer.
The information on this page is based on research about trans women, but some of it will be relevant to non-binary and intersex people who’ve had gender affirming surgery or are taking feminising hormones.
Tests for trans women at the GP surgery
The tests you have will depend on your medical history and any medicines you’re taking. Some of the test results will be interpreted differently if you’re taking feminising hormones. These include oestrogen or drugs that block the effect of testosterone (testosterone blockers or anti-androgens).
But the tests you have for prostate cancer will be similar to the tests in cis men – even if you’ve had gender affirming surgery or you’re taking feminising hormones.
You might have a urine test, a blood test and a prostate examination at your GP surgery. Your GP may then refer you to a doctor at the hospital who specialises in urinary problems (a urologist), for more information and tests if necessary.
You can also discuss any worries you may have with a doctor at an NHS gender dysphoria clinic, who can refer you to a urologist.
PSA blood test in trans women
The PSA blood test helps to diagnose prostate problems, including prostate cancer. Trans women have the same right to a PSA blood test as cis men.
You have the right to a test if you have thought carefully about the advantages and disadvantages - you need to make an appointment with your doctor to talk about these. The test is carried out for free on the NHS.
If you have not yet medically transitioned and are over 50 (or over 45 if you're Black or have a family history), ask about getting a PSA blood test before you start taking feminising hormones or have the testicles removed (orchidectomy). Read more about the risk factors and getting tested.
If you’ve had feminising hormones or an orchidectomy, then what’s considered a normal PSA level for you will be lower than for cis men.
In trans women, a normal PSA is:
- under 3ng/ml if you’ve not had feminising hormones or an orchidectomy
- under 1ng/ml if you have had feminising hormones or an orchidectomy.
A raised PSA level doesn’t mean you definitely have prostate cancer. It is the first step in deciding if you need more tests, such as a magnetic resonance imaging (MRI) scan. To find out more, read our general information about the PSA blood test.
Prostate examination
Sometimes, a doctor may ask to do a physical check of your prostate using a finger. If you have had a vaginoplasty (surgery to form a vagina), then your prostate can be examined through your vagina.
You might have to explain this to your doctor if they don’t know you’ve had a vaginoplasty. You could also show them the diagram below.
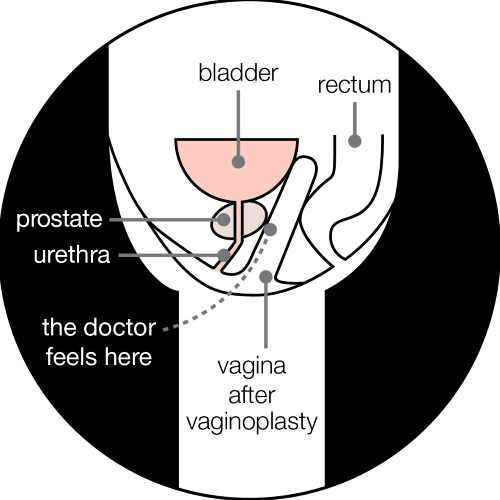
If you have not had a vaginoplasty, then you can have a digital rectal examination. This is where a doctor feels your prostate through the wall of your back passage (rectum).
You don’t have to have a physical examination of your prostate to check for prostate cancer. You can choose to only have a PSA blood test, followed by other tests to confirm the diagnosis.
Tests for trans women at the hospital
After tests at your GP surgery, you might be referred for more tests at the hospital urology clinic. This might be a general urology clinic attended by cis men and cis women, or a prostate cancer clinic attended only by cis men. Ask your doctor what to expect.
When you arrive at the clinic for your appointment, take your referral letter to the receptionist. They should treat you with courtesy and refer to you by name. You do not have to explain your reasons for attending the clinic to the reception staff, or to any other patients there.
Some trans women and non-binary and intersex people find it uncomfortable to wait in a room full of cis men. If you are worried, here are some tips that may help.
- When you arrange your appointment, ask if you can have it at the beginning or end of the clinic when it might be quieter.
- Call the clinic ahead of your appointment to ask about the waiting room arrangements. You might be able to attend a clinic that has a mixed waiting room.
- Consider taking someone with you, or have a book or magazine to read while you wait for your appointment.
- At the start of your appointment, discuss the language and pronouns the doctor should use for you.
- Prepare what you would like to discuss. Read about speaking to a health professional about prostate problems as a trans woman. You could also download our checklist for talking to your GP about prostate cancer.
MRI scan
An MRI scan would be carried out in the same way as for a cis man. Read more about what an MRI scan involves. You might have to wait a few weeks for a scan if you’ve recently had gender affirming surgery.
Biopsy
There are three types of biopsy:
- trans-rectal ultrasound (TRUS) guided biopsy
- transperineal biopsy
- transvaginal biopsy.
The urologist will look at your MRI scans before deciding on the best approach. They will discuss this with you before carrying out the procedure.
If you’ve had a vaginoplasty, then you may have a transvaginal biopsy, where a thin needle goes through the wall of the vagina. This might depend on the level of experience the urologist has in carrying out the procedure through the vagina.
If you have not had a vaginoplasty, then you will likely have a TRUS guided biopsy, where a thin needle goes through the wall of the back passage. Or you may have a transperineal biopsy, where a thin needle goes through the skin between the genitals and back passage (the area known as the perineum).
Speaking to a health professional about prostate cancer
If you’re a trans woman, or a non-binary or intersex person who identifies with femininity, you might feel uncomfortable talking to your GP about possible prostate problems. You might worry that you’ll be ‘outed’ or treated as male. You might also feel anxious about having tests, and fear that they will be invasive.
Remember that conversations with health professionals are confidential, and they are required to treat you with respect. This should include:
- writing the correct names and pronouns on your records
- addressing you correctly at reception, and during treatments and appointments
- making alternative arrangements where possible to make you feel more comfortable.
Your doctor should not share your trans history with other healthcare professionals, or anyone else, without your permission. But you may want to give them permission, so you don’t have to keep explaining it to other healthcare professionals.
Read more about your right to be treated equally to everyone else. If your GP says they don’t know as much about prostate problems in trans women, then they have a duty of care to find out more. You could suggest they contact an NHS gender dysphoria clinic or the UK Cancer and Transition Service (UCATS) for expert guidance.
It’s important that you feel comfortable with your GP. If you feel uncomfortable for any reason, you’re allowed to ask to see someone else and you do not have to explain why. You could ask to see another GP in the same practice, or register with a new practice.
What to say to your GP
Start by explaining that you’re aware you have a prostate and are at risk of prostate cancer – even if your risk is lower than it is for cis men.
It’s very important to mention any symptoms or risk factors you have, such as a family history of prostate cancer. You don’t have to reveal your trans history to your GP unless you want to, but it will help them give you the best care.
Not all of your medical history is relevant to your prostate health, but some information can affect your diagnosis and treatment – such as how long you’ve been taking feminising hormones and any surgery you’ve had.
Many health professionals won’t have seen a trans woman with a prostate problem before (or any trans people at all), so you might need to play a role in educating them. If your GP is unsure, they can contact an NHS gender dysphoria clinic or the UK Cancer and Transition Service (UCATS) for expert guidance.
If you’re worried about starting a conversation with your GP about prostate problems, consider taking our checklist for talking to your GP about prostate cancer to your appointment. You could also show your GP some of the information about trans women on our website.
Getting support for prostate problems as a trans woman
Prostate Cancer UK’s services are free and open to everyone. Partners and family members can also use our services.
Our health information
On our website, we have other information for trans women on:
Our Specialist Nurses
Our Specialist Nurses can answer your questions and explain your diagnosis and treatment options. All our Specialist Nurses can provide sensitive and appropriate support and information to trans women and non-binary people assigned male at birth.
Our online community
Our online community is a place to talk about whatever’s on your mind – your questions, your ups and your downs. Anyone can ask a question or share an experience.
The online community is open to all, and we have a dedicated section for trans women. Here, you can talk to others who may share or understand your experiences of prostate cancer and other prostate problems.
Who else can help?
Clinical services
The UK Cancer and Transition Service (UCATS) is an NHS clinic that supports trans and non-binary people affected by cancer. The service aims to help you manage your cancer and gender affirming care. There is also signposting to further support, and you can find out how to get involved in research.
If you have been diagnosed with prostate cancer, you can refer yourself to UCATS, or your doctor or nurse can refer you.
UCATS is part of TransPlus, which is a gender, sexual health and HIV service.
Support groups
At support groups, you can share your experiences of living with prostate cancer. You can also ask questions and share worries, knowing that people will understand what you’re going through.
These are support groups for gay and bisexual men with prostate cancer who also encourage trans women and non-binary and intersex people to attend:
OUTpatients provides support groups for any LGBTIQ+ person with and beyond cancer. They host regular peer support meetings and workshops, and have a strong transgender representation.
Organisations
You may also find it helpful to contact organisations that support trans, intersex and non-binary people, such as:
References and reviewers
Updated: April 2025. To be reviewed: April 2028.
- Bertoncelli Tanaka M, Sahota K, Burn J, et al. Prostate cancer in transgender women: what does a urologist need to know? BJU Int. 2022;129(1):113-122. doi:10.1111/bju.15521
- Braybrook D, Bristowe K, Timmins L, et al. Communication about sexual orientation and gender between clinicians, LGBT+ people facing serious illness and their significant others: a qualitative interview study of experiences, preferences and recommendations. BMJ Qual Saf. 2023;32(2):109-120. doi:10.1136/bmjqs-2022-014792
- Crowley F, Mihalopoulos M, Gaglani S, et al. Prostate cancer in transgender women: considerations for screening, diagnosis and management. Br J Cancer. 2023;128(2):177-189. doi:10.1038/s41416-022-01989-y
- Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102(11):3869-3903. doi:10.1210/jc.2017-01658
- Manfredi C, Ditonno F, Franco A, et al. Prostate Cancer in Transgender Women: Epidemiology, Clinical Characteristics, and Management Challenges. Curr Oncol Rep. Published online November 1, 2023. doi:10.1007/s11912-023-01470-w
- NHS patients’ rights. Citizens Advice. Accessed March 24, 2025. https://www.citizensadvice.org.uk/scotland/health/nhs-healthcare-s/nhs-patients-rights-s/
- Nik-Ahd F, De Hoedt AM, Butler C, et al. Prostate-Specific Antigen Values in Transgender Women Receiving Estrogen. JAMA. 2024;332(4):335-337. doi:10.1001/jama.2024.9997
- Nik-Ahd F, Jarjour A, Figueiredo J, et al. Prostate-Specific Antigen Screening in Transgender Patients. Eur Urol. 2023;83(1):48-54. doi:10.1016/j.eururo.2022.09.007
- The NHS Constitution for England. GOV.UK. Accessed March 24, 2025. https://www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england
- Alison Berner, Honorary Consultant and Academic Clinical Lecturer in Medical Oncology, Specialty Doctor in Adult Gender Identity Medicine, Queen Mary University of London/Barts Health NHS Trust/Chelsea & Westminster Hospitals NHS Foundation Trust
- Ashley d’Aquino, Lecturer Practitioner, The Royal Marsden NHS Foundation Trust
- Katherine Read, Radiotherapy Review Radiographer, The Royal Marsden NHS Foundation Trust
- Laura Hinchliffe, Clinical Director, Cardiff Local Gender Service
- Oliver Hulson, Consultant Radiologist, Leeds Cancer Centre
- Shaina Tennant, Medical Writer, Wallace Health: wallacehealth.co.uk/
- Stewart O'Callaghan, Founder & Chief Executive Officer, OUTpatients: https://outpatients.org.uk/
- Our Specialist Nurses
- Our Volunteers.

