Role of NHS in raising awareness about prostate cancer risk
Practical guidance to address earlier diagnosis and tackling health inequalities
Supporting our NHS
We’d like to support our primary and secondary care colleagues in achieving better outcomes for men at risk of prostate cancer and ensuring NHS goals related to early cancer diagnosis and CORE20PLUS5 and the health inequalities agenda are achieved.
-
NHS Long Term Plan sets out key ambitions for 75% of cancers to be diagnosed at early stages 1 and 2 by 2028.
-
CORE20PLUS5 addresses health inequalities targeting those in the most deprived areas, with one of the plus5 areas of focus being early cancer diagnosis.
-
Primary Care Network DES contract specification 2025/26 emphasises the importance of collaboration and working with external partners to achieve their goals.
Health inequalities
In areas where there is high deprivation and/or Black communities, we know that health outcomes are poorer for these men. We provide guidance on how you can begin to improve these outcomes for men.

Many GPs are unaware that the risks of harm to patients referred onto secondary care have reduced significantly. Men are now scanned first and then go onto biopsy, which means more than 30% drop out of the pathway at the first test. The way that men are biopsied has changed as well, with many areas conducting trans perineal biopsies vs trans rectal biopsies reducing the risk of sepsis.
Don’t be a blocker
It’s important that admin staff when triaging calls with asymptomatic men, or GPs when having conversations with their patients don’t become blockers to accessing PSA blood tests.
There is growing awareness of men’s risk to prostate cancer, men are becoming informed and for some, want to have a PSA test once aware of the pros and cons of the test.
Men should be able to access these tests if they have made this informed decision, particularly if they are Black and have a family history due to their higher risk.
This change in approach, will begin to engage and build trust in communities which may have had poor experiences in accessing appointments and ultimately, help to improve health outcomes for your patients.
We would also recommend clinical staff engaging with local community groups, attending events to share risk awareness messaging, promoting health information accessibility, to build trust and to share the message that they matter.
Also refer to our Engaging with Black Communities toolkit for further insights
Please use this content to help support your work and get in touch with us to discuss how we can support you with engaging with Black communities, resources, CPD education packages and opportunities to train non-HCPs on risk awareness.
One of the biggest issues that we found, was around the use of the digital rectal examination. 3 out of 5 men, told us that they’d be concerned about having “the finger up the bum” and that this was one of the biggest barriers for them to go to their GP to talk about their prostate health. We found that this changed when men are told that the first step to being diagnosed is with the PSA blood test.
We’re aware that in some areas, a rectal exam may occur if PSA readings are high. We’d recommend reviewing your use of the DRE and our article in the British Journal of General Practioners provides more detail on its use as a screening tool. Men should be made aware that they can refuse having this test if they wish.
Action:
1. Review your use of the DRE if it’s in place in your area.
2. Order and provide men at risk information with our z cards on prostate cancer and what the PSA blood test is.
3. Create a notice board with information about the prostate, PSA blood tests and order our posters on 1 in 8 / 1 in 4 risk to Black/men.
4. Organise a community event with grass root charities, ensuring clinical staff attend to support messaging to at risk groups and to help enlist trusted members of communities to pass on messaging.
Letting men know that the first test to understanding their prostate health is a simple blood test is a great way of addressing the misconceptions around what the test is. We advocate that GPs and other health care professionals are proactive in having conversations with men at risk, to share information about their risk and to let them know about the PSA blood test along with its pros and cons.
This will help to address health literacy issues, digital exclusion through online information and the existing health inequalities that affect men having the confidence to talk to their GP about their risk and request a PSA blood test.
Action
1. Let men at risk know about their risk and that the first test is a simple blood test.
2. Ensure that staff the PSA blood test is a term that’s adopted by your clinical and admin staff when talking to men about what the test is.
3. Avoid using scary language that includes number of deaths – our behavioural insights showed that this creates anxiety and stops men from taking action.
Prostate cancer is the most common cancer for men with 1 in 8 men being diagnosed with it and for Black men, this doubles to 1 in 4. Through our research, we found that 74% of men couldn’t identify what their prostate does. This lack of knowledge about the prostate needs to be addressed and NHS stakeholders should be proactive in providing accurate information so that men are able to make informed choices about their prostate health.
Action
1. Order and provide men aged 50+ information with our quick guide on prostate cancer and what the PSA blood test is.
2. Organise an awareness event with local grass roots charities as recommended in the PCN DES to provide information. This does not have to be exclusively about prostate health.
Messaging about many cancers focuses on symptoms and for patients to be vigilant for things like blood in their wee, a persistent cough and so on. However, we know that for prostate cancer and earlier diagnosis, a focus on symptoms is not helpful. Indeed, only 1 in 3 men knew that early-stage prostate cancer has no symptoms.
This is why we advocate that men should be aware of their risk and can make informed decisions about whether they want to have a PSA blood test. We found that 3 in 5 men won’t bother their GP if they don’t have symptoms. A shift in approach needs to happen to ensure that men are aware of their risk and messaging needs to be clear, that they should not wait for symptoms to speak to their GP.
Action
1. Have proactive conversations with men at high risk about their prostate cancer risk and let them know about the PSA blood test.
2. Order our resources to provide to these men.
Our research found that 1 in 2 men believed that they would be invited to have a test if they were at risk. We can assume from this that these men will therefore not be proactive with their health seeking behaviours. This is of concern, since as we know those who only seek medical advice when/if they start having symptoms could affect stage of diagnosis, treatment choices and survival rates.
Action
1. HCPs have proactive conversations with their at risk men about their risk levels and that they have the option of having a PSA blood test if they are concerned once they have received information about the pros and cons of the test in a balanced, non biased way.
Who to target
Adopting a risk stratified approach will target the right people to have conversations with.

Talking to your patients
Once you've identified your at risk population, create an alert on their records, so that when these men attend surgery, you can have a conversation with them about their risk of prostate cancer and address the above. This can be done in the style of a very brief advice (VBA) session that typically happens for smokers.
- Admin staff should identify these patients whilst booking their appointments and create an alert for the GP pre appointment.
- GPs can use the below sample to help structure a very brief conversation:
“We are speaking to men over 45 who are Black / men over 50 , to provide information about their potential prostate cancer risk. Would you like to speak to someone in the surgery about this?”
- If the patient would like to be sent some information, check you have their up-to-date mobile number and send the above text that includes our risk checker.
- Alternatively order our hard copy resources using the links at the bottom of this webpage.
To evaluate the impact of your intervention, we recommend that you either create your own SNOMED code or use the below code. This will help for when you come to audit patients who have been contacted and to detail their patient journey.
It is important to:
1. Check that the SNOMED code is currently not in use
2. Ensure that all practices in your PCN/area consistently use this code.
3. Embed the SNOMED codes into the text messaging template system that you are using.
Patient advised about prostate cancer screening (situation)
SCTID: 698470001
698470001 | Patient advised about prostate cancer screening (situation) |
Advice given about prostate cancer screening
Patient advised about prostate cancer screening
Patient advised about prostate cancer screening (situation)
You can download this process on a flowchart to present at meetings and to help support staff.
1. Discuss the approach that your primary care/project team will adopt to raise awareness about prostate cancer risk, how you will have conversations with men, health clinics, flagging men at risk, community engagement etc. Use this content to help define outputs, metrics and evaluation.
2. Work out who will lead on your earlier diagnosis/health inequalities work –a clinical lead / cancer champion / an admin member of staff.
3. Collaborate: You may also want to consider working with grass roots charities within your area, to engage with communities, share messaging and explore holding a health event as part of your health inequalities work. We can also support you with this work, particularly if engaging with Black communities, with resources and guidance.
4. Once you’ve decided who’ll do this work, let staff know that men without symptoms may well start contacting the surgery asking about the PSA blood test or to speak to a GP, ensuring that they have access to a GP/PSA blood test if that is what they want.
Your next step is to conduct an audit on how many of your patients fall within the risk categories. We’d recommend prioritising in the below order based on their risk.
1. Black men aged 45-69
2. Men with a family history of prostate, breast, or ovarian cancer aged 45-69
3. Men aged 50-69
Men should be excluded if they:
- Have a diagnosis of prostate cancer
- Have had a PSA blood test within the last 12-months
- Are on an end-of-life / palliative care pathway
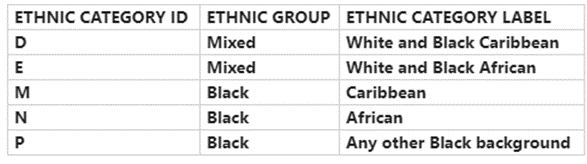
We would recommend that when considering searching for your patients who are Black men, the below ethnic categories are used.
If you’re interested in getting your own specific trackable risk checker link, then please contact us.
All we need to know is the name of your surgery/PCN.
We have a number of resources that you can order for events / handing to patients. Please see our website for more information.
Action I’d like to request risk checker link
What's worked well nationally
There are a number of pilot programmes that have made access for men at risk to trained healthcare professionals easier so that they can discuss their prostate cancer risk and to access having the PSA blood test.
• Bristol and London primary care prostate cancer case finding – British Journal Of General Practice (2024)
• Prostate cancer case finding project – Surrey and Sussex Cancer Alliance
• Improving access to specialists and tests – University Hospital Southampton
• Man in Van project – Greater Manchester Cancer Alliance
• Man in Van project – Royal Marsden Cancer Alliance
• Prostate Cancer UK’s innovation event on PCN-DES 2023
We’ve also worked with health stakeholders nationally and have showcased these projects in online innovation events with talks from the clinical/cancer/project leads.
• Health inequalities – Learn what different areas are doing to tackle health inequalities and finding men at risk of prostate cancer
• National projects on how to reach men at risk including our Bristol pilot
• Innovative projects from PCNs about their risk awareness activities
• Extended access: Offering access to PSA blood tests on a Saturday morning clinic has proven to be effective, whilst also offering other health checks. This will help to target men at work and those who can’t get to a surgery between Monday-Friday.
• Use Patient Participation Groups to distribute posters in communities, shops, barbers, etc.
• Run your event in locations where you know your at risk population frequent, eg, local church, community centre, shopping centre etc.
Evaluate your project
There are a couple of ways in which you will be able to measure the impact of your work:
1. Use the above SNOMED code and complete an audit in 6 months time, to review the number of conversations had with men at risk.
2. Further evaluation can include the number of PSA tests completed, number of Faster Diagnosis referrals made and number of diagnoses.
3. Risk checker data – if we’ve created a bespoke URL for your work, we’ll be able to tell you the number of risk checker completions, number of men who are in the three risk categories and if they decide that they can make an informed decision about their health.
Role and responsibilities of NHS in raising awareness about prostate cancer risk
We provide information on what's required from NHS stakeholders in improving health outcomes for men.
Get in touch
Projects and Support
If you require support in setting up your project then please contact us.
Educational support – find out about courses, CPD, resources.



