Enlarged prostate
An enlarged prostate is an increase in the size of the prostate. It isn’t caused by cancer. The medical term for an enlarged prostate is benign prostatic enlargement (BPE).
- Benign – not cancer.
- Prostatic – to do with the prostate.
- Enlargement – an increase in size.
You might also hear it called benign prostatic hyperplasia (BPH). Hyperplasia means an increase in the number of cells. It is this increase in cells that makes the prostate grow bigger (see diagram below). In our information, we use the words 'enlarged prostate' to describe both BPE and BPH.
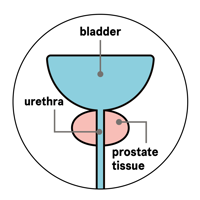
A normal prostate
A enlarged prostate
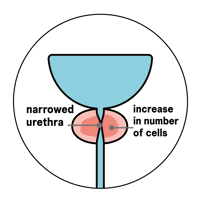
An enlarged prostate is very common in men over the age of about 50. It can affect younger men too, although this is uncommon. Not everyone with an enlarged prostate get symptoms. But as the prostate grows, it can press on the outside of the urethra, causing the urethra to become narrow. This can slow down or sometimes even stop the flow of urine when you try to urinate.
About 1 in 3 men over the age of 50 have urinary symptoms. The most common cause of these symptoms is an enlarged prostate.
Enlarged prostate: A guide to diagnosis and treatment
This booklet is for men who want to know more about a condition called an enlarged prostate. You may also hear it called benign prostatic enlargement (BPE) or benign prostatic hyperplasia (BPH).
Our Specialist Nurse, John, answers some common questions about an enlarged prostate. He explains the symptoms, how it’s diagnosed and how it may be treated.
What causes an enlarged prostate?
We still don’t really know all the things that cause the prostate to grow. But we do know about two risk factors that can increase your risk of having an enlarged prostate.
Age
Your risk of having an enlarged prostate increases as you get older. Many men aged 50 or over have an enlarged prostate, but they don’t all get symptoms. And some men have symptoms that don't bother them.
Hormone levels
The balance of hormones (oestrogen and testosterone) in your body changes as you get older. This may cause your prostate to grow.
Other factors
Some studies show that obese men and men who have diabetes may be more likely to develop an enlarged prostate. Regular exercise may help to reduce your risk of urinary symptoms. But we still need more studies into the causes of enlarged prostate to know for certain if, and how, we can prevent it.
There is also some research that suggests you may be more at risk of developing an enlarged prostate if your father or brother has one. Again, further studies are needed to confirm this.
What are the symptoms?
An enlarged prostate is the most common cause of urinary problems in men as they get older. Possible symptoms include:
- a weak flow when you urinate
- a feeling that your bladder hasn’t emptied properly
- difficulty starting to urinate
- dribbling urine after you finish urinating
- needing to urinate more often, especially at night
- a sudden urge to urinate – you may sometimes leak before you get to the toilet.
You may not get all of these symptoms, and some men with an enlarged prostate don’t get any symptoms at all. These symptoms can also be caused by other things, such as cold weather, anxiety, other health problems, lifestyle factors, and some medicines. If you have any symptoms, visit your GP to find out what may be causing them.
Blood in your urine may be a symptom of an enlarged prostate. But this is rare and is usually caused by something else. Tell your doctor if you have blood in your urine.
Am I more likely to get prostate cancer if I have an enlarged prostate?
No, having an enlarged prostate does not increase your risk of getting prostate cancer. The two problems usually begin in different parts of the prostate. But men can have an enlarged prostate and prostate cancer at the same time.
If you’re worried about prostate cancer, talk to your GP or call our Risk Information Service.
How might an enlarged prostate affect my life?
Having an enlarged prostate affects everyone in different ways. Some men can manage mild symptoms and don’t need treatment. Others find they need to stay near a toilet. This can make it difficult to work, drive, be outdoors and attend social events. If you need the toilet a lot during the night, this can affect your sleep and make you feel more tired during the day.
Some men find their symptoms improve over time without treatment. But for most, the symptoms will stay the same or slowly start to cause more problems over time unless they have treatment.
What other problems might an enlarged prostate cause?
A small number of men may find it difficult to empty their bladder properly – this is called urine retention. If you’ve been diagnosed with an enlarged prostate, your doctor will look at your test results to see if you’re at risk of urine retention. You may be more likely to get urine retention if:
- you’re aged 70 or over
- your prostate is very large
- you have a raised prostate specific antigen (PSA) level
- you have severe urinary symptoms and a very slow flow.
Chronic urine retention
This is where you can’t empty your bladder fully, but can still urinate a little. It usually develops slowly over time. Chronic means long-lasting. The first signs often include a weak flow when you urinate, or leaking urine at night. You may feel that your abdomen (stomach area) is swollen, or that you’re not emptying your bladder fully.
Chronic urine retention is usually painless. But the pressure of the urine can slowly stretch your bladder muscle and make it weaker. This can cause urine to be left behind in the bladder when you urinate. If you don’t empty your bladder fully, you might get a urine infection, need to urinate more often, leak urine at night, or get painful bladder stones. You might also see some blood in your urine. Chronic urine retention can damage your bladder and kidneys if it isn’t treated.
There are several treatments for chronic urine retention, including:
- passing a thin, flexible tube called a catheter to drain urine from your bladder
- medication
- surgery to widen the urethra.
Acute urine retention
This is when you suddenly and painfully can’t urinate at all. It needs treating straight away. If this happens, call your doctor or nurse, or go to your nearest accident and emergency (A&E) department. They may need to drain your bladder using a catheter. Before the catheter is removed, you may be offered a medicine called an alpha-blocker. This may help stop you getting acute retention again.
How is an enlarged prostate diagnosed?
Some tests for an enlarged prostate can be done at your GP surgery. Your GP might also arrange for you to see a doctor who specialises in urinary problems (a urologist) or a specialist nurse at the hospital.
What are the treatment options?
There are three main types of treatment for an enlarged prostate:
- lifestyle changes
- medicines
- surgery.
Read our information on treatment for an enlarged prostate.
References
Updated: September 2025 | Due for Review: September 2026
- Cahn DB, Ross CP, Dubowitch EP, Persun ML, Ginsberg PC, Harkaway RC. Predicting Acute Urinary Retention in Patients with Elevated Post-Void Residuals. Current Urology. 2015 Jul;8(2):79–83.
- Cho A, Chughtai B, Te AE. Benign Prostatic Hyperplasia and Male Lower Urinary Tract Symptoms: Epidemiology and Risk Factors. Curr Bladder Dysfunct Rep. 2020 Jun;15(2):60–5.
- Devlin CM, Simms MS, Maitland NJ. Benign prostatic hyperplasia – what do we know? BJU Int. 2021 Apr;127(4):389–99.
- Egan KB. The Epidemiology of Benign Prostatic Hyperplasia Associated with Lower Urinary Tract Symptoms. Urologic Clinics of North America. 2016 Aug;43(3):289–97.
- Gudmundsson J, Sigurdsson JK, Stefansdottir L, Agnarsson BA, Isaksson HJ, Stefansson OA, et al. Genome-wide associations for benign prostatic hyperplasia reveal a genetic correlation with serum levels of PSA. Nat Commun. 2018 Dec;9(1):4568.
- Huang SW, Tsai CY, Tseng CS, Shih MC, Yeh YC, Chien KL, et al. Comparative efficacy and safety of new surgical treatments for benign prostatic hyperplasia: systematic review and network meta-analysis. BMJ. 2019 Nov 14;l5919.
- Jarvis TR, Chughtai B, Kaplan SA. Bladder Outlet Obstruction and BPH. Curr Bladder Dysfunct Rep. 2014 Dec;9(4):372–8.
- Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis. Sci Rep. 2017 Dec;7(1):7984.
- Lim KB. Epidemiology of clinical benign prostatic hyperplasia. Asian Journal of Urology. 2017 Jul;4(3):148–51.
- Madersbacher S, Sampson N, Culig Z. Pathophysiology of Benign Prostatic Hyperplasia and Benign Prostatic Enlargement: A Mini-Review. Gerontology. 2019;65(5):458–64.
- Management of Urinary Retention in Patients with Benign Prostatic Obstruction: A Systematic Review and Meta-analysis | Elsevier Enhanced Reader [Internet]. [cited 2021 Nov 26]. Available from: https://reader.elsevier.com/reader/sd/pii/S0302283819300922?token=11A2599BEEDEDAE22939E53046B67D23532F392058A5DD79C5AF74FF923DB89811415D83C6BA8A8FA54CB046B5D9EBC7&originRegion=eu-west-1&originCreation=20211126122948
- National Institute for Health and Care Excellence. Lower urinary tract symptoms in men: management. 2015; Available from: https://www.nice.org.uk/guidance/cg97
- Ørsted DD, Bojesen SE. The link between benign prostatic hyperplasia and prostate cancer. Nat Rev Urol. 2013 Jan;10(1):49–54.
- Raheem OA, Parsons JK. Associations of obesity, physical activity and diet with benign prostatic hyperplasia and lower urinary tract symptoms: Current Opinion in Urology. 2014;24(1):10–4.
- Rees J, Bultitude M, Challacombe B. The management of lower urinary tract symptoms in men. BMJ. 2014 Jun 24;348(1):g3861–g3861.
- Russo GI, Castelli T, Urzì D, Privitera S, La Vignera S, Condorelli RA, et al. Emerging links between non-neurogenic lower urinary tract symptoms secondary to benign prostatic obstruction, metabolic syndrome and its components: A systematic review. International Journal of Urology. 2015;22(11):982–90.
- Schenk JM, Kristal AR, Arnold KB, Tangen CM, Neuhouser ML, Lin DW, et al. Association of Symptomatic Benign Prostatic Hyperplasia and Prostate Cancer: Results from the Prostate Cancer Prevention Trial. American Journal of Epidemiology. 2011;173(12):1419–28.
- Sellers J, Wagstaff RG, Helo N, de Riese WTW. Quantitative measurements of prostatic zones by MRI and their dependence on prostate size: possible clinical implications in prostate cancer. Therapeutic Advances in Urology. 2021 Jan;13:175628722110008.
- Shah A, Shah AA, K N, Lobo R. Mechanistic targets for BPH and prostate cancer–a review. Reviews on Environmental Health. 2021 Jun 25;36(2):261–70.
- Speakman M, Kirby R, Doyle S, Ioannou C. Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH) – focus on the UK. BJU International. 2015;115(4):508–19.
- Stefanova I, Currie AC, Newton RC, Albon L, Slater G, Birnie A, et al. Systematic Review and Meta-Analysis of the Impact of Bariatric Surgery on Lower Urinary Tract Symptoms in Males. OBES SURG. 2021 Jul;31(7):3151–8.
- Vickman RE, Franco OE, Moline DC, Vander Griend DJ, Thumbikat P, Hayward SW. The role of the androgen receptor in prostate development and benign prostatic hyperplasia: A review. Asian Journal of Urology. 2020 Jul;7(3):191–202.
- Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016 Feb;13(2):108–19.
- Wynder JL, Nicholson TM, DeFranco DB, Ricke WA. Estrogens and Male Lower Urinary Tract Dysfunction. Curr Urol Rep. 2015 Sep;16(9):61.
- Yoon PD, Chalasani V, Woo HH. Systematic review and meta-analysis on management of acute urinary retention. Prostate Cancer Prostatic Dis. 2015 Dec;18(4):297–302.
This publication was reviewed for accuracy and updated by:
- our health information team
- our Specialist Nurses.


