Developing a blood test to spot prostate cancers at risk of coming back

Grant information
Reference: RIA24-ST2-011
Lead researcher: Professor Yong-Jie Lu
Institution: Queen Mary University of London
Award: £588,576
What you need to know
- Some cancers that seem to be contained within the prostate come back after surgery because a small number of cancer cells spread before treatment – too small to spot with scans.
- This study looks at blood samples to find these hidden cells and how the immune system responds to them, aiming to predict which men are most at risk of their cancer returning.
- A simple blood test could help doctors choose the best treatment, avoiding unnecessary surgery and improving survival.
Why are we funding this research?
If prostate cancer is caught early enough, surgery can be a cure. But for some of these men the cancer ‘comes back’, because tiny clusters of cancer cells, too small to detect, escape the prostate before surgery and start growing elsewhere. This means these men have to undergo further treatment.
This research is building a new kind of blood test that could reduce the risk of this happening, spotting these cells before they cause a problem. This could help doctors decide which men would do well on surgery alone and who might need extra treatment.
What makes this project different is that it’s combining several clues from the blood – including cancer cells, DNA fragments from dead cells, and immune signals – to get a clearer picture of what’s really going on.
What will the researchers do?
This project aims to improve our understanding of why prostate cancer sometimes comes back after surgery, and to look for ways to predict this in advance.
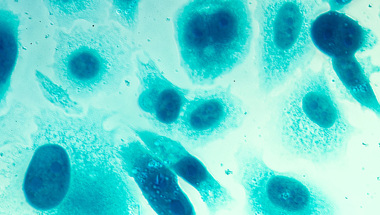
The researchers believe the answer lies in tiny cancer cells that escape into the bloodstream before surgery – too small to be seen on scans. These cells, called circulating tumour cells (CTCs), can quietly settle elsewhere in the body and cause the cancer to return.
To tackle this, the team will study blood samples from over 200 men who’ve already had surgery and are now being monitored for signs that their cancer has returned.
The team will look for CTCs in these samples, but also go a step further by checking how the men’s immune system is reacting. That’s because a strong immune response might destroy leftover cancer cells (a sign these men might not need further treatment to get rid of them), while a weaker one might let them grow.
The team will also look for fragments of cancer DNA floating in the blood – another clue that cancer cells are active. By combining all this information with data collected on which of the 200 men’s cancers did and didn’t come back after surgery, the researchers hope to spot patterns that can predict this recurrence.
The goal is to develop a simple blood test that can guide treatment decisions. If the test shows a man’s cancer is unlikely to return, he might be able to avoid extra treatment. But if the test suggests a man is at higher risk, doctors could offer him added treatments early on. It’s about giving men the best chance of a cure, while avoiding unnecessary side effects.
With this funding from Prostate Cancer UK, we’re developing a blood test to help choose the best treatment for men whose cancer looks contained. By studying cancer cells and immune signals in the blood, we hope to improve outcomes and reduce unnecessary side effects for men.
How will this benefit men?
Right now, even when scans suggest the cancer hasn’t spread, it can still come back after surgery.
By developing a blood test that picks up these hidden cells and shows how the immune system is responding, this study could help spot who’s at risk of recurrence. That means men who don’t need extra treatment could avoid it, and those who do need it could get it sooner – before the cancer has a chance to grow again.
It’s about making treatment more personal. Instead of a one-size-fits-all approach, doctors could tailor care based on what’s really happening inside the body. In the long run, this could give men longer lives with fewer side effects, and more confidence in the choices they and their doctors make.
Help us fund more research like this
Your donation helps us fund lifesaving research that's improving the way we diagnose and treat prostate cancer.