Reducing health inequalities by using new tools to find more effective treatments for Black men

Grant information
Reference: RIA24-ST2-006
Lead researcher: Professor Craig Robson and Dr Adriana Buskin
Institution: Newcastle University
Award: £497,055
What you need to know
- Black men are more likely to get prostate cancer, often at a younger age and with more aggressive disease. Yet most research is based on white men, leaving big gaps in our understanding.
- The team will use cells from Black men to grow mini-tumours in the lab, enabling them to study two key genes that are linked to prostate cancer and more likely to be faulty in Black men.
- They'll also look at whether existing treatments for other conditions could be repurposed to target these genetic changes, paving the way for fairer, more effective treatments.
Why are we funding this research?
Black men are more likely to develop prostate cancer than white men, and the disease is often more aggressive. Yet most of what we know about prostate cancer comes from studies on white men. This means we don’t fully understand why Black men are at higher risk or how best to treat them. That lack of knowledge contributes to health inequalities.
We do know that two genes, called SPOP and BRCA2, are more likely to be faulty in prostate cancers found in Black men. When these genes don’t work properly, they can make cancer grow faster. But current lab models don’t reflect these genetic differences, so researchers can’t easily test which treatments might work best.
This project aims to change that, and could lead to fairer, more effective treatments and help close the gap in outcomes.
What will the researchers do?
Firstly, the researchers will take prostate cells donated by Black men and reprogram them into stem cells. These special cells can grow into many other types of cell, including prostate cells.
Using a gene editing tool, the team will then make changes to two genes (called SPOP and BRCA2) that are often faulty in prostate cancers found in Black men. These faults make it harder for cells to repair DNA damage, which can drive cancer growth.
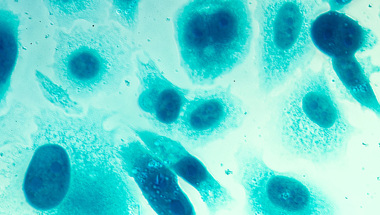
The team will then grow these genetically edited cells in 3D, creating lab-grown ‘mini-tumours’ known as organoids. These are more accurate representations of an actual prostate cancer tumour than the traditional approach of growing cells flat in a dish.
The researchers will then use these organoids to study how these gene changes affect the way prostate cells behave. They’ll also test a range of existing drugs, including some already used for other cancers, to see if any can be repurposed to target these weaknesses. Because these drugs are already approved for use in people, they could move into clinical trials more quickly.
Finally, the researchers will analyse genetic data from thousands of Black men with prostate cancer to look for other important changes that might influence how their cancers respond to treatment.
We're developing new pre-clinical models that more accurately reflect how prostate cancer affects Black men. This work aims to address the urgent need to understand why Black men are twice as likely to develop prostate cancer, a disparity that existing models – largely based on white men – fail to explain.
How will this benefit men?
This research could lead to fairer, more effective treatments for men whose prostate cancer is driven by specific genetic changes.
At the moment, most treatments are based on studies in white men, which means they may not work as well for everyone. By creating new lab models that reflect the biology of Black men, the researchers can test which drugs work best for cancers with changes in two key genes, SPOP and BRCA2.
And, because the researchers will focus on drugs that already exist, any successful findings could move into clinical trials more quickly.
In the long term, this work could help doctors choose treatments based on the genetic make-up of a man’s cancer, rather than a one-size-fits-all approach. That means better outcomes, fewer side effects, and a real step towards reducing the health gap between Black men and white men.
Help us fund more research like this
Your donation helps us fund lifesaving research that's making prostate cancer care fairer for everyone.