Research
31 Aug 2023Behind the headlines: could MRI be used to screen men for prostate cancer?
Last week, newspapers reported that a 10-minute MRI scan could cut prostate cancer deaths ‘significantly’. We go behind the headlines to find out what this could mean for men.

Research suggesting MRI scans could be used to screen men for prostate cancer has recently attracted widespread interest.
The research was featured in papers including The Times and The Guardian, as well as on Sky News and BBC News. So, let’s look at the research and what we’ve learned from it.
What is a screening programme?
A screening programme is a way to test people who have no symptoms to see if they have a health condition, or if they are more likely to get one in future.
The NHS routinely screens people for some cancers, including breast cancer and bowel cancer, but there is currently no screening programme for prostate cancer.
Because prostate cancer often doesn’t show any symptoms in its early stages – when it is easiest to cure – a screening programme for the disease could save thousands of lives. Currently, more than 10,000 men each year in the UK are diagnosed too late for a cure.
Why is there no screening programme for prostate cancer?
Unfortunately, there is currently no one test that can pick out which men have prostate cancer and rule out those who do not.
The PSA blood test, which is usually the first step towards a diagnosis, isn’t accurate enough to tell by itself if a man has prostate cancer or not. A high PSA level can be caused by a range of other things, such as exercise, sex and urine infections. And some men can develop prostate cancer without having a high PSA level.
That’s why we are working to find a test, or combination of tests, that might be suitable to screen men in future.
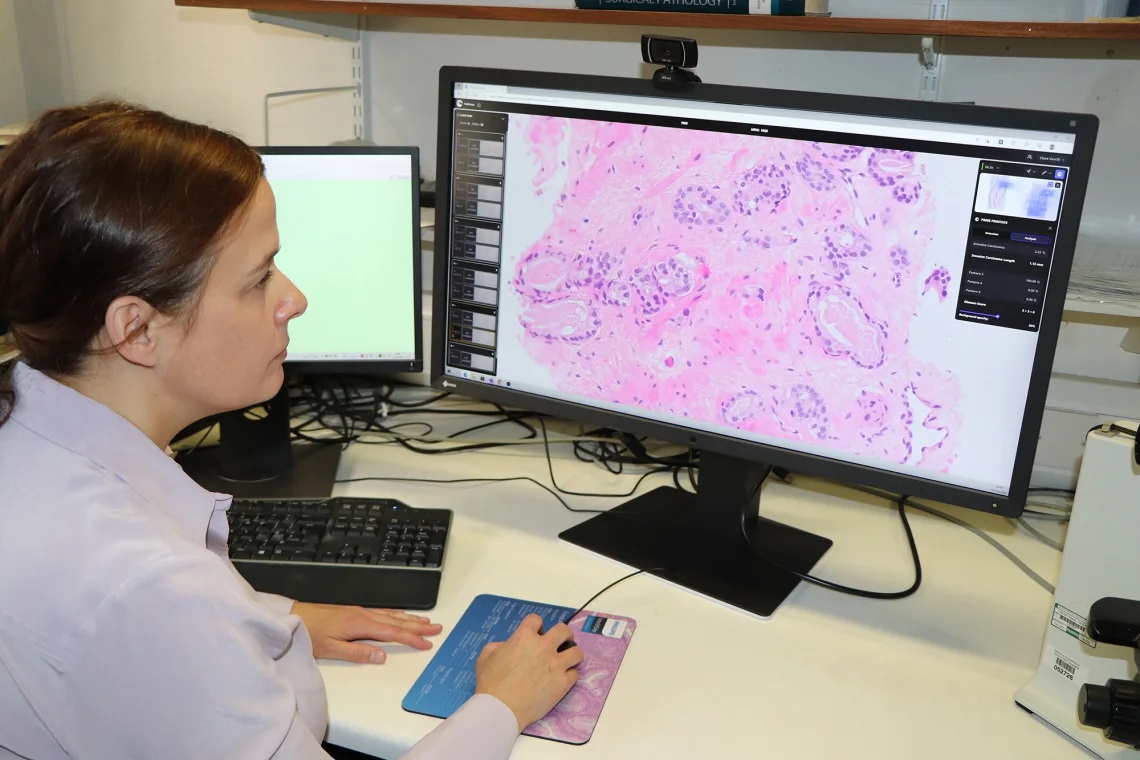
Our support was instrumental in building the evidence to underpin the use of MRI in men with a raised PSA level. More recently, our research has shown that the inclusion of these MRI scans, as well as safer biopsy procedures, in the diagnosis process is tipping the balance in favour of screening. What's more, research we’ve funded has explored how we might further increase the accuracy of MRI scans to safely rule out prostate cancer without the need for a biopsy.
What did the researchers do?
For this study, published in the journal BMJ Oncology, researchers invited men aged 50 to 75 to have a screening MRI and a PSA blood test.
Out of the 303 men who took both tests, 64 were flagged by either the MRI scan or the PSA blood test as having potential prostate cancer.
These men were referred for further tests on the NHS, and 29 of them (45%) were found to have prostate cancer that needed treatment, while a further three men (5%) had low-risk cancer that did not need treating.
However, there was a big difference between the MRI results and the PSA blood test results.
The MRI scans picked up 25 out of the 29 serious prostate cancers, while the PSA blood test picked up just 14 – meaning that more than half of the cancers would have been missed by a PSA blood test alone.
Professor Caroline Moore, consultant surgeon at University College London Hospital and chief investigator of the study, said: “The thought that half the men with clinically significant cancer would have been reassured that they didn’t have cancer by a PSA test alone is a sobering one and reiterates the need to consider a new approach to prostate cancer screening.
“Our results give an early indication that MRI could offer a more reliable method of detecting potentially serious cancers early, with the added benefit that less than 1 per cent of participants were ‘over-diagnosed’ with low-risk disease. More studies in larger groups are needed to assess this further.”

Why can’t we just roll out MRI screening now?
Although the research is exciting, the trial screened only a small number of men – 303 – and just 29 of these had prostate cancer that needed treatment. A much bigger study is now needed to see if this accuracy holds up across a larger population of men before it could be rolled out across the whole country.
What’s more, although Black men’s risk of prostate cancer is double that of other men, just 13 of the men screened were Black – and none had an MRI scan that suggested potential cancer. This means it is hard to tell from these results if Black men would see the same benefit from an MRI-based screening programme and highlights the importance of future larger studies being much more representative of the UK population.
Simon Grieveson, Assistant Director of Research at Prostate Cancer UK, said: “MRI scans have revolutionised the way we diagnose prostate cancer, and it’s great to see research into how we might use these scans even more effectively.
“These results are extremely exciting, and we now want to see much larger, UK-wide studies to understand if using MRI as the first step in getting tested could form the basis of a national screening programme.”
What is Prostate Cancer UK doing to make a screening programme happen?
Right now, we have been working closely with the research community to work out what research is needed to provide the definitive evidence to support a screening programme, and how to deliver it.
We recently asked for researchers to submit their proposals for funding a large-scale trial that would get the evidence the health service would need to roll out regular testing for prostate cancer. While we are in the early stages of establishing this study, we are committed to supporting the research required to transform how we diagnose prostate cancer.
Simon Grieveson said: “We desperately need screening to help us catch more cancers early and save thousands of men’s lives each year — that’s why Prostate Cancer UK is committed to funding the vital research needed to make a national screening programme a reality, so that every man who’s at risk gets tested as early as possible.”
We’ll continue to update supporters on research developments as we work towards a screening programme for prostate cancer in the UK.