Treating very small tumours with targeted radiotherapy to prevent recurrence

Grant information
Researcher: Dr Edward O’Neill
Institution: University of Oxford
Grant award: £299,271
Reference: TLD-CAF22-003
What you need to know
- Dr O’Neill is studying new kind of radiation treatment for prostate cancer called 177Lu-PSMA.
- This treatment can deliver radiation to cancer cells that have spread beyond the prostate to other parts of the body.
- Dr O’Neill wants to see if this new treatment can also work on really small groups of cancer cells that are too small to be seen with PET or CT scans.
About Dr O’Neill
Dr O'Neill completed his PhD at the University of Sydney, where he studied MRI contrast agents – a type of dye that can be injected into a person to make their MRI scans clearer. For his postdoctoral research he moved into nuclear imaging – again, a way of making scans clearer, this time by using radioactive compounds that are drawn to cancer cells and can be picked up on PET or CT scans. This led to his interest in lutetium, the focus of this project.
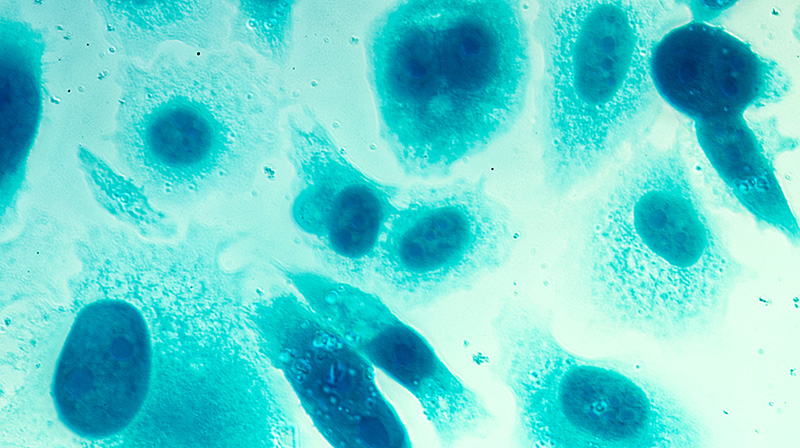
During his fellowship, Dr O’Neill will travel to Monash University in Melbourne, Australia. There, he will work with Professor Gail Risbridger and Professor Renea Taylor to develop his skills in creating lab-grown tumours (known as organoids) from samples taken from men with prostate cancer.
With these skills, he will be well-placed to test new ideas and develop new treatments, and be able to set up his own research team to take his ideas further.
These seek-and-destroy treatments are becoming more widespread throughout the UK. My research will identify promising drug combinations for clinical evaluation and provide much needed understanding to how these radiation treatments work.
What will Dr O’Neill do?
Dr O’Neill wants to study a new kind of radiation treatment for prostate cancer called 177Lu-PSMA. Unlike traditional radiotherapy, which uses x-rays from outside the body, this treatment uses a small, targeted dose of radiation inside the body. It combines a radioactive part (an element called lutetium, or 177Lu for short), with another part that detects a protein (called PSMA) found in prostate cancer cells.
By combining these two parts, the treatment essentially finds prostate cancer cells throughout the body and exposes them to radiation so that they die.
We know from clinical trials that 177Lu-PSMA can be used for advanced prostate cancer, where the cancer cells have spread beyond the prostate and formed tumours elsewhere. It was recently approved in the US for this.
But Dr O’Neill thinks the treatment could also be useful for men at an earlier stage, before these tumours are large enough to appear on scans. Even when a man has early-stage prostate cancer, some small groups of cancer cells, called micrometastases, may exist beyond the prostate. If these are not caught, they may eventually develop into larger tumours, even if the original cancer is removed. This mean that stopping micrometastases early, using 177Lu-PSMA, could stop prostate cancer from coming back (recurrence).
Because it is hard to see these micrometastases on scans, there is currently little evidence about how effective 177Lu-PSMA would be at stopping them. It is also possible that the micrometastases will be too small to draw enough 177Lu-PSMA to themselves to make a difference. With this research project, Dr O’Neill hopes to collect the evidence that could lead to clinical trials one day.
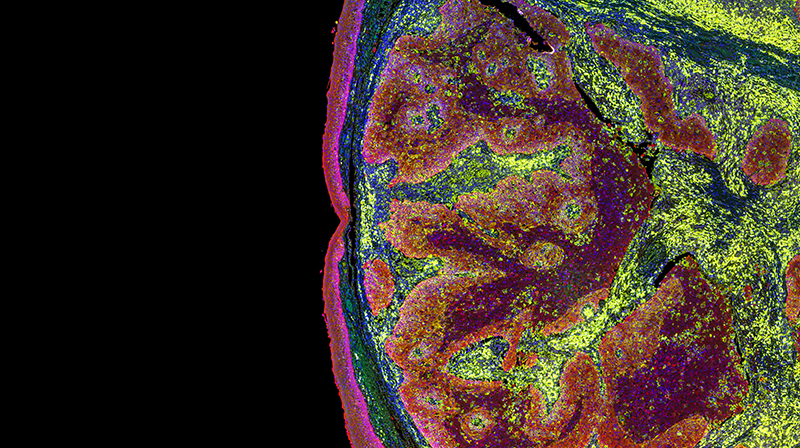
To do this, he will use something called organoids, which are small clumps of cancer cells grown in the lab to about the size of micrometastases. He will treat the organoids with 177Lu-PSMA to see if it will work on tumours this small. He will also see if the treatment is more effective alongside an extra drug that makes cells more sensitive to radiation.
How will this benefit men?
If Dr O’Neill can show that 177Lu-PSMA can be used to treat micrometastases, it could be a big help for men with prostate cancer. Targeting these small groups of cancer cells would make existing treatments more effective by keeping the cancer from spreading or returning. This could lead to better outcomes for men with prostate cancer and help them live longer, healthier lives.
Help us fund more research like this
Your donation helps us fund lifesaving research into better treatments for prostate cancer.