Advanced prostate cancer
What is advanced prostate cancer?
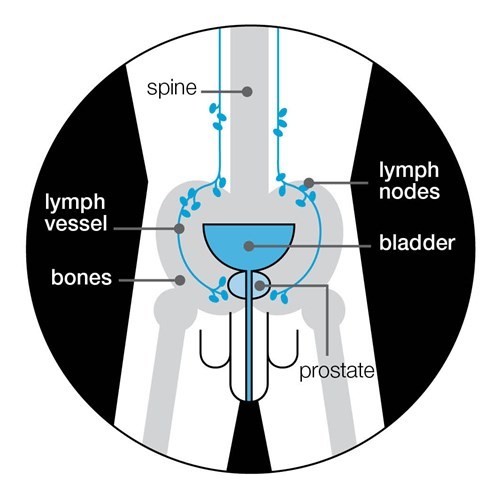
Advanced prostate cancer is cancer that has spread from the prostate to other parts of the body. It develops when prostate cancer cells move through the blood stream or lymphatic system.
Watch our video about advanced prostate cancer.
You might hear cancer that has spread described as metastatic prostate cancer, secondary prostate cancer, secondaries, metastases or mets. It is still prostate cancer, wherever it is in the body.
Prostate cancer can spread to any part of the body, but most commonly to the bones and lymph nodes. Lymph nodes (sometimes called lymph glands) are part of your lymphatic system, which is part of the body’s immune system. Lymph nodes are found throughout the body including in the pelvic area, near the prostate.
Advanced prostate cancer can cause symptoms, such as fatigue (extreme tiredness), bone pain, and problems urinating.
The symptoms you have will depend on where the cancer has spread to. Speak to your doctor or nurse if you have any symptoms. There are treatments available to help manage them.
It’s not possible to cure advanced prostate cancer. But treatments can help keep it under control and manage any symptoms.
Read more about symptoms and treatments to help manage them.
How is advanced prostate cancer diagnosed?
Advanced prostate cancer is diagnosed using the results of some or all of the following tests:
What do my test results mean?
Your results will give your doctor an idea of where your cancer has spread to. This will help you and your doctor to discuss which treatments might be suitable for you.
What treatments are available?
If you have advanced prostate cancer, treatment won’t cure your cancer. But it can help keep it under control and manage any symptoms.
If you’ve just been diagnosed with advanced prostate cancer, you may be offered the following treatments:
- hormone therapy
- chemotherapy with hormone therapy
- clinical trials.
If you’ve just been diagnosed with advanced prostate cancer, you may be offered a type of radiotherapy called external beam radiotherapy as part of your first treatment. Research has found that having radiotherapy together with one of the main treatments listed above can help some men with advanced prostate cancer to live longer. But radiotherapy isn’t suitable for all men with advanced prostate cancer. Speak to your doctor or nurse to find out if radiotherapy is suitable for you.
New (second-generation hormone therapy)
There are newer types of hormone therapy that can be used to treat some men with advanced prostate cancer. They may be used in combination with first line hormone therapy treatment, or when your prostate cancer has stopped responding other types of hormone therapy. They include abiraterone (Zytiga®) and enzalutamide (Xtandi®).
If you live in Scotland, abiraterone acetate (Zytiga®) is routinely available, as a first treatment, together with standard hormone therapy. If you live in England, Wales or Northern Ireland, you'll probably be offered a different type of hormone therapy called enzalutamide. But if you get severe side effects, you may then be offered abiraterone instead.
Triplet therapy
Triplet therapy is a new treatment. It combines the hormone therapy, darolutamide (Nubeqa®) with both standard hormone therapy and chemotherapy (docetaxel). Triplet therapy is a treatment for men with newly diagnosed hormone-sensitive advanced prostate cancer. This means your prostate cancer has spread to other parts of the body but can be treated with hormone therapy. Read more about triplet therapy.
Before you start treatment
Before you start any treatment, make sure you have all the information you need. It’s important to think about how you would cope with the possible side effects. Speak to your doctor or nurse about this.
It can help to write down any questions you want to ask at your next appointment. It may also help to take someone with you, such as your partner, a family member or friend.
It can also help to write down or record what’s said to help you remember it. You have the right to record your appointment because it’s your personal data. You could use your phone or another recording device to do this. Let your doctor or nurse know why you are doing this, as not everyone is comfortable being recorded.
If you have any questions, speak to our Specialist Nurses.
If you don’t have any symptoms and want to avoid or delay treatment and its side effects, you might be able to have your cancer monitored instead. This is known as watchful waiting. It isn’t usually recommended for men with advanced prostate cancer, because it won’t control the cancer and it won’t stop the cancer from growing or spreading. Your doctor or nurse can help you think about the advantages and disadvantages.
How will my cancer be monitored?
Your doctor will talk to you about how often you should have check-ups. At some hospitals, you may not have many appointments at the hospital itself. Instead, you may talk to your doctor or nurse over the telephone. You might hear this called self-management.
You will have regular PSA tests. This is often a useful way to check how well your treatment is working. You’ll also have regular blood tests to see whether your cancer is affecting other parts of your body, such as your liver, kidneys or bones.
You might have more scans to see how your cancer is responding to treatment and whether your cancer is spreading.
Your doctor or nurse will also ask you how you’re feeling and if you have any symptoms, such as pain or tiredness. This will help them understand how you’re responding to treatment and how to manage any symptoms. Let them know if you have any side effects from your treatment. There are usually ways to manage these.
What happens if my cancer starts to grow again?
Your first treatment may help keep your cancer under control. But over time, the cancer may change and it may start to grow again.
You will usually stay on your first type of hormone therapy, even if it’s not working so well. This is because it will still help to keep the amount of testosterone in your body low. But there are other treatments that you can have alongside your usual treatment, to help control the cancer and manage any symptoms. Other treatments include:
- more hormone therapy
- more chemotherapy
- radium-223 (Xofigo®)
- olaparib (Lynparza®️)
- clinical trials
Which treatments are suitable for me?
Which treatments are suitable for you will depend on many things, including your general health, how your cancer responds to treatment, and which treatments you’ve already had. Talk to your doctor or nurse about your own situation, or speak to our Specialist Nurses.
Treatments to help manage symptoms
Advanced prostate cancer can cause symptoms, such as bone pain. Speak to your doctor or nurse if you have symptoms – there are treatments available to help manage them. The treatments above may help to delay or relieve some symptoms. There are also specific treatments to help manage symptoms – you may hear these called palliative treatments. They include:
Your multi-disciplinary team (MDT)
This is the team of health professionals involved in your care. It is likely to include:
- a specialist nurse
- a chemotherapy nurse
- a urologist (a surgeon who specialises in diseases of the urinary and reproductive systems, including prostate cancer)
- an oncologist (a doctor who specialises in cancer treatments other than surgery)
- a radiologist (a doctor who reads scans such as MRI, CT and bone scans)
- other health professionals, such as a dietitian or physiotherapist.
Your MDT will meet to discuss your diagnosis and treatment options. You might not meet all the health professionals straight away.
Your main point of contact might be called your key worker. This is usually your clinical nurse specialist (CNS), but might be someone else. The key worker will co-ordinate your care and help you get information and support. You may also have close contact with your GP and the practice nurses at your GP surgery.
What is my outlook?
If you’re diagnosed with advanced prostate cancer, you may want to know how well your treatment is likely to control your cancer and for how long it will control it. This is sometimes called your outlook or prognosis. But not all men will want to know this.
While it isn’t possible to cure advanced prostate cancer, treatments can help keep it under control, often for several years. Treatments will also help manage any symptoms, such as pain.
No one can tell you exactly what your outlook will be, as it will depend on many things such as where the cancer has spread to, how quickly it has spread, and how well you respond to treatment. Some men may not respond well to one treatment, but may respond better to another. And if your first treatment stops working, there are other treatments available to help keep the cancer under control for longer. Speak to your doctor about your own situation and any questions or concerns you have.
Questions to ask your doctor or nurse
- What type of hormone therapy are you offering me and why?
- Are there other treatments I can have?
- What are the advantages and disadvantages of my treatment?
- What treatments and support are available to help manage side effects?
- Are there any lifestyle changes that might help me manage my cancer, symptoms, or side effects?
- How often will I have check-ups and what will this involve?
- How will we know if my cancer starts to grow again?
- What other treatments are available if that happens?
- Can I join any clinical trials?
- If I have any questions or get any new symptoms, who should I contact?
References
Updated: April 2023|To be reviewed: April 2026
- Abiraterone acetate (Zytiga) [Internet]. Scottish Medicines Consortium. [cited 2022 Apr 25]. Available from: https://www.scottishmedicines.org.uk/medicines-advice/abiraterone-acetate-zytiga-full-smc2215/
- Abrahamsen B, Brask-Lindemann D, Rubin KH, Schwarz P. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. BoneKEy Rep. 2014 Sep 3;3:574.
- Abrahamsson PA. Intermittent androgen deprivation therapy in patients with prostate cancer: Connecting the dots. Asian J Urol. 2017 Oct;4(4):208–22.
- Ahmadi H, Daneshmand S. Androgen deprivation therapy: evidence-based management of side effects. BJU Int. 2013 Apr;111(4):543–8.
- Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. The Lancet. 2017 Jan;
- Allott EH, Masko EM, Freedland SJ. Obesity and Prostate Cancer: Weighing the Evidence. Eur Urol. 2013 May;63(5):800–9.
- Botrel TEA, Clark O, dos Reis RB, Pompeo ACL, Ferreira U, Sadi MV, et al. Intermittent versus continuous androgen deprivation for locally advanced, recurrent or metastatic prostate cancer: a systematic review and meta-analysis. BMC Urol. 2014;14:9.
- Bourke L, Smith D, Steed L, Hooper R, Carter A, Catto J, et al. Exercise for Men with Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol. 2016 Apr;69(4):693–703.
- Cancer Research UK. Prostate cancer survival by stage at diagnosis [Internet]. Cancer Research UK. 2016 [cited 2019 Mar 29]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/survival
- Cheung AS, Zajac JD, Grossmann M. Muscle and bone effects of androgen deprivation therapy: current and emerging therapies. Endocr Relat Cancer. 2014 Sep 17;21(5):R371–94.
- Chipperfield K, Brooker J, Fletcher J, Burney S. The impact of physical activity on psychosocial outcomes in men receiving androgen deprivation therapy for prostate cancer: A systematic review. Health Psychol. 2014;33(11):1288–97.
- Cimadamore A, Lopez-Beltran A, Massari F, Santoni M, Mazzucchelli R, Scarpelli M, et al. Germline and somatic mutations in prostate cancer: focus on defective DNA repair, PARP inhibitors and immunotherapy. Future Oncol [Internet]. 2020 Jan 9 [cited 2021 Oct 14]; Available from: https://www.futuremedicine.com/doi/abs/10.2217/fon-2019-0745
- Colloca G, Venturino A, Governato I, Checcaglini F. Incidence and Correlates of Fatigue in Metastatic Castration-Resistant Prostate Cancer: A Systematic Review. Clin Genitourin Cancer. 2016 Feb;14(1):5–11.
- Cormie P, Newton RU, Taaffe DR, Spry N, Joseph D, Hamid MA, et al. Exercise maintains sexual activity in men undergoing androgen suppression for prostate cancer: a randomized controlled trial. Prostate Cancer Prostatic Dis. 2013;16(2):170–5.
- Crawley D, Garmo H, Rudman S, Stattin P, Häggström C, Zethelius B, et al. Association between duration and type of androgen deprivation therapy and risk of diabetes in men with prostate cancer. Int J Cancer. 2016;139(12):2698–704.
- Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer. 2011 Nov 8;105:S52–73.
- de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med. 2020 May 28;382(22):2091–102.
- de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010 Oct 2;376(9747):1147–54.
- De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, et al. Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporos Int. 2005 Nov;16(11):1330–8.
- Dong Z, Wang H, Xu M, Li Y, Hou M, Wei Y, et al. Intermittent hormone therapy versus continuous hormone therapy for locally advanced prostate cancer: a meta-analysis. Aging Male. 2015 Dec;18(4):233–7.
- Dorff TB, Crawford ED. Management and challenges of corticosteroid therapy in men with metastatic castrate-resistant prostate cancer. Ann Oncol. 2013 Jan 1;24(1):31–8.
- Drudge-Coates L, Oh WK, Tombal B, Delacruz A, Tomlinson B, Ripley AV, et al. Recognizing Symptom Burden in Advanced Prostate Cancer: A Global Patient and Caregiver Survey. Clin Genitourin Cancer. 2018 Apr 1;16(2):e411–9.
- Edmunds K, Tuffaha H, Galvão DA, Scuffham P, Newton RU. Incidence of the adverse effects of androgen deprivation therapy for prostate cancer: a systematic literature review. Support Care Cancer. 2020 May 1;28(5):2079–93.
- Elliott S, Latini DM, Walker LM, Wassersug R, Robinson JW. Androgen Deprivation Therapy for Prostate Cancer: Recommendations to Improve Patient and Partner Quality of Life: Improving Life on ADT. J Sex Med. 2010 Sep;7(9):2996–3010.
- Fagerlund A, Cormio L, Palangi L, Lewin R, Santanelli di Pompeo F, Elander A, et al. Gynecomastia in Patients with Prostate Cancer: A Systematic Review. PLoS ONE [Internet]. 2015 Aug 26 [cited 2018 Sep 12];10(8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4550398/
- Gagliano-Jucá T, Travison TG, Nguyen PL, Kantoff PW, Taplin ME, Kibel AS, et al. Effects of Androgen Deprivation Therapy on Pain Perception, Quality of Life, and Depression in Men With Prostate Cancer. J Pain Symptom Manage. 2018 Feb 1;55(2):307-317.e1.
- Gardner JR, Livingston PM, Fraser SF. Effects of Exercise on Treatment-Related Adverse Effects for Patients With Prostate Cancer Receiving Androgen-Deprivation Therapy: A Systematic Review. J Clin Oncol. 2014 Feb 1;32(4):335–46.
- General Medical Council. Confidentiality: Good practice in handling patient information [Internet]. 2017. Available from: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/confidentiality
- Ghadjar P, Aebersold DM, Albrecht C, Böhmer D, Flentje M, Ganswindt U, et al. Treatment strategies to prevent and reduce gynecomastia and/or breast pain caused by antiandrogen therapy for prostate cancer. Strahlenther Onkol. 2020;196(7):589–97.
- Hamilton K, Chambers SK, Legg M, Oliffe JL, Cormie P. Sexuality and exercise in men undergoing androgen deprivation therapy for prostate cancer. Support Care Cancer. 2015 Jan;23(1):133–42.
- Haseen F, Murray LJ, Cardwell CR, O’Sullivan JM, Cantwell MM. The effect of androgen deprivation therapy on body composition in men with prostate cancer: Systematic review and meta-analysis. J Cancer Surviv. 2010 Jun 1;4(2):128–39.
- Hechtman LM. Clinical Naturopathic Medicine [Internet]. Harcourt Publishers Group (Australia); 2014 [cited 2015 Jul 21]. 1610 p. Available from: http://www.bookdepository.com/Clinical-Naturopathic-Medicine-Leah-Hechtman/9780729541923
- Husson O, Mols F, Poll-Franse LV van de. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Ann Oncol. 2010 Sep 24;mdq413.
- Islami F, Moreira DM, Boffetta P, Freedland SJ. A Systematic Review and Meta-analysis of Tobacco Use and Prostate Cancer Mortality and Incidence in Prospective Cohort Studies. Eur Urol. 2014 Dec;66(6):1054–64.
- James ND, Spears MR, Clarke NW, Dearnaley DP, De Bono JS, Gale J, et al. Survival with Newly Diagnosed Metastatic Prostate Cancer in the “Docetaxel Era”: Data from 917 Patients in the Control Arm of the STAMPEDE Trial (MRC PR08, CRUK/06/019). Eur Urol. 2015 Jun;67(6):1028–38.
- James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. The Lancet. 2016 Mar;387(10024):1163–77.
- Jhan JH, Yeh HC, Chang YH, Guu SJ, Wu WJ, Chou YH, et al. New-onset diabetes after androgen-deprivation therapy for prostate cancer: A nationwide propensity score-matched four-year longitudinal cohort study. J Diabetes Complications. 2018 Jul;32(7):688–92.
- Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med [Internet]. 2018 Mar 18 [cited 2018 May 4]; Available from: http://www.nejm.org/doi/10.1056/NEJMoa1801993
- Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, et al. Effects of resistance exercise in prostate cancer patients: a meta-analysis. Support Care Cancer. 2017 Jun 10;
- Keto CJ, Aronson WJ, Terris MK, Presti JC, Kane CJ, Amling CL, et al. Obesity is associated with castration-resistant disease and metastasis in men treated with androgen deprivation therapy after radical prostatectomy: results from the SEARCH database. BJU Int. 2011;110(4):492–8.
- Kim TJ, Koo KC. Pathophysiology of Bone Loss in Patients with Prostate Cancer Receiving Androgen-Deprivation Therapy and Lifestyle Modifications for the Management of Bone Health: A Comprehensive Review. Cancers. 2020 Jun 10;12(6):1529.
- Langston B, Armes J, Levy A, Tidey E, Ream E. The prevalence and severity of fatigue in men with prostate cancer: a systematic review of the literature. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. 2013 Jun;21(6):1761–71.
- Larkin D, Lopez V, Aromataris E. Managing cancer-related fatigue in men with prostate cancer: A systematic review of non-pharmacological interventions. Int J Nurs Pract. 2014 Oct;20(5):549–60.
- Lynparza 100mg Film-Coated Tablets - Summary of Product Characteristics (SmPC) - (emc) [Internet]. [cited 2021 Oct 14]. Available from: https://www.medicines.org.uk/emc/product/9204/smpc
- Lynparza 150mg Film-Coated Tablets - Summary of Product Characteristics (SmPC) - (emc) [Internet]. [cited 2021 Oct 14]. Available from: https://www.medicines.org.uk/emc/product/9488/smpc
- Lynparza [Internet]. European Medicines Agency. 2018 [cited 2021 Oct 26]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/lynparza
- Magnan S, Zarychanski R, Pilote L, Bernier L, Shemilt M, Vigneault E, et al. Intermittent vs Continuous Androgen Deprivation Therapy for Prostate Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2015 Sep 17;1–10.
- Meng F, Zhu S, Zhao J, Vados L, Wang L, Zhao Y, et al. Stroke related to androgen deprivation therapy for prostate cancer: a meta-analysis and systematic review. BMC Cancer [Internet]. 2016 Dec [cited 2019 Jan 25];16(1). Available from: http://bmccancer.biomedcentral.com/articles/10.1186/s12885-016-2221-5
- Messina C, Cattrini C, Soldato D, Vallome G, Caffo O, Castro E, et al. BRCA Mutations in Prostate Cancer: Prognostic and Predictive Implications. J Oncol. 2020 Sep 7;2020:4986365.
- Moreira DM, Aronson WJ, Terris MK, Kane CJ, Amling CL, Cooperberg MR, et al. Cigarette smoking is associated with an increased risk of biochemical disease recurrence, metastasis, castration-resistant prostate cancer, and mortality after radical prostatectomy: Results from the SEARCH database. Cancer. 2014 Jan 15;120(2):197–204.
- Mottet N, Cornford P, van der Bergh RCN. EAU Guidelines on Prostate Cancer. European Association of Urology; 2022.
- Muniyan S, Xi L, Datta K, Das A, Teply BA, Batra SK, et al. Cardiovascular risks and toxicity - the Achilles heel of androgen deprivation therapy in prostate cancer patients. Biochim Biophys Acta Rev Cancer. 2020 Aug;1874(1):188383.
- Myint ZW, Momo HD, Otto DE, Yan D, Wang P, Kolesar JM. Evaluation of Fall and Fracture Risk Among Men With Prostate Cancer Treated With Androgen Receptor Inhibitors. JAMA Netw Open. 2020 Nov 17;3(11):e2025826.
- National Institute for Clinical Excellence. Suspected cancer: recognition and referral [Internet]. 2021. Available from: https://www.nice.org.uk/guidance/ng12
- National Institute for Health and Care Excellence. Abiraterone for treating metastatic hormone-relapsed prostate cancer before chemotherapy is indicated. Technology appraisal guidance 387. 2016.
- National Institute for Health and Care Excellence. Cabazitaxel for hormone-relapsed metastatic prostate cancer treated with docetaxel. Technology appraisal guidance 391. 2016.
- National Institute for Health and Care Excellence. Docetaxel for the treatment of hormone-refractory metastatic prostate cancer. NICE technology appraisal guidance 101. 2006.
- National Institute for Health and Care Excellence. Enzalutamide for treating hormone-sensitive metastatic prostate cancer [Internet]. 2021. Available from: https://www.nice.org.uk/guidance/ta712
- National Institute for Health and Care Excellence. Overview | Apalutamide with androgen deprivation therapy for treating hormone-sensitive metastatic prostate cancer | Guidance | NICE [Internet]. NICE; 2021 [cited 2021 Nov 2]. Available from: https://www.nice.org.uk/guidance/ta741
- National Institute for Health and Care Excellence. Patient experience in adult NHS services: improving the experience of care for people using adult NHS services. 2021.
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management [Internet]. 2021 [cited 2022 Dec 19]. Available from: https://www.nice.org.uk/guidance/ng131
- National Institute for Health and Care Excellence. Radium-223 dichloride for treating hormone-relapsed prostate cancer with bone metastases. Technology appraisal guidance 412 [Internet]. 2016 [cited 2016 Oct 26]. Available from: https://www.nice.org.uk/guidance/ta412/chapter/1-Recommendations
- National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. NICE guideline 12 [Internet]. 2020. Available from: https://www.nice.org.uk/guidance/ng12
- Nead KT, Sinha S, Yang DD, Nguyen PL. Association of androgen deprivation therapy and depression in the treatment of prostate cancer: A systematic review and meta-analysis. Urol Oncol Semin Orig Investig. 2017 Nov 1;35(11):664.e1-664.e9.
- Newby TA, Graff JN, Ganzini LK, McDonagh MS. Interventions that may reduce depressive symptoms among prostate cancer patients: a systematic review and meta-analysis. Psychooncology. 2015 Dec;24(12):1686–93.
- Nguyen PL, Alibhai SMH, Basaria S, D’Amico AV, Kantoff PW, Keating NL, et al. Adverse Effects of Androgen Deprivation Therapy and Strategies to Mitigate Them. Eur Urol. 2015 May;67(5):825–36.
- NHS Choices. The risks of drinking too much [Internet]. 2017 [cited 2017 Jul 4]. Available from: http://www.nhs.uk/Livewell/alcohol/Pages/Effectsofalcohol.aspx
- NHS England. Clinical Commissioning Policy Statement: Docetaxel in combination with androgen deprivation therapy for the treatment of hormone naive metastatic prostate cancer. 2016.
- Oefelein MG, Ricchuiti V, Conrad W, Seftel A, Bodner D, Goldman H, et al. Skeletal fracture associated with androgen suppression induced osteoporosis: the clinical incidence and risk factors for patients with prostate cancer. J Urol. 2001;166(5):1724–8.
- olaparib (Lynparza) [Internet]. Scottish Medicines Consortium. [cited 2021 Oct 26]. Available from: https://www.scottishmedicines.org.uk/medicines-advice/olaparib-lynparza-full-smc2366/
- Owen PJ, Daly RM, Livingston PM, Fraser SF. Lifestyle guidelines for managing adverse effects on bone health and body composition in men treated with androgen deprivation therapy for prostate cancer: an update. Prostate Cancer Prostatic Dis. 2017 Jun;20(2):137–45.
- Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fosså SD, et al. Alpha Emitter Radium-223 and Survival in Metastatic Prostate Cancer. N Engl J Med. 2013;369(3):213–23.
- Parker CC, James ND, Brawley CD, Clarke NW, Hoyle AP, Ali A, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. The Lancet. 2018 Oct;
- Pettersson A, Johansson B, Persson C, Berglund A, Turesson I. Effects of a dietary intervention on acute gastrointestinal side effects and other aspects of health-related quality of life: A randomized controlled trial in prostate cancer patients undergoing radiotherapy. Radiother Oncol. 2012 Jun;103(3):333–40.
- Public Health England. Prostate cancer risk management programme (PCRMP): benefits and risks of PSA testing [Internet]. GOV.UK; 2016. Available from: https://www.gov.uk/government/publications/prostate-cancer-risk-management-programme-psa-test-benefits-and-risks/prostate-cancer-risk-management-programme-pcrmp-benefits-and-risks-of-psa-testing
- Ryan CW, Huo D, Stallings JW, Davis RL, Beer TM, McWhorter LT. Lifestyle Factors and Duration of Androgen Deprivation Affect Bone Mineral Density of Patients with Prostate Cancer During First Year of Therapy. Urology. 2007 Jul;70(1):122–6.
- Sayegh N, Swami U, Agarwal N. Recent Advances in the Management of Metastatic Prostate Cancer. JCO Oncol Pract. 2022 Jan;18(1):45–55.
- Saylor PJ, Smith MR. Metabolic Complications of Androgen Deprivation Therapy for Prostate Cancer. J Urol. 2013 Jan;189(1):S34–44.
- Scottish Medicines Consortium. Cabazitaxel, 60mg concentrate and solvent for solution for infusion (Jevtana®). SMC No.735/11. 2016.
- Serpa Neto A, Tobias-Machado M, Esteves MAP, Senra MD, Wroclawski ML, Fonseca FLA, et al. Bisphosphonate therapy in patients under androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2012;15(1):36–44.
- Singer EA, Srinivasan R. Intravenous therapies for castration-resistant prostate cancer: Toxicities and adverse events. Urol Oncol Semin Orig Investig. 2012 Jul;30(4):S15–9.
- Song P, Huang C, Wang Y. The efficacy and safety comparison of docetaxel, cabazitaxel, estramustine, and mitoxantrone for castration-resistant prostate cancer: A network meta-analysis. Int J Surg. 2018 Aug 1;56:133–40.
- Teyssonneau D, Margot H, Cabart M, Anonnay M, Sargos P, Vuong NS, et al. Prostate cancer and PARP inhibitors: progress and challenges. J Hematol OncolJ Hematol Oncol. 2021 Mar 29;14(1):51.
- Tillisch K. Complementary and alternative medicine for functional gastrointestinal disorders. Gut. 2006 May 1;55(5):593–6.
- Tucci M, Bertaglia V, Vignani F, Buttigliero C, Fiori C, Porpiglia F, et al. Addition of Docetaxel to Androgen Deprivation Therapy for Patients with Hormone-sensitive Metastatic Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol. 2015 Sep;
- Vale CL, Burdett S, Rydzewska LH, Albiges L, Clarke NW, Fisher D, et al. Addition of docetaxel or bisphosphonates to standard of care in men with localised or metastatic, hormone-sensitive prostate cancer: a systematic review and meta-analyses of aggregate data. Lancet Oncol. 2015;
- van der Zande K, Oyen WJG, Zwart W, Bergman AM. Radium-223 Treatment of Patients with Metastatic Castration Resistant Prostate Cancer: Biomarkers for Stratification and Response Evaluation. Cancers. 2021 Aug 27;13(17):4346.
- Walker LM, Santos-Iglesias P, Robinson J. Mood, sexuality, and relational intimacy after starting androgen deprivation therapy: implications for couples. Support Care Cancer. 2018 May 18;1–8.
- Wedlake LJ, Shaw C, Whelan K, Andreyev HJN. Systematic review: the efficacy of nutritional interventions to counteract acute gastrointestinal toxicity during therapeutic pelvic radiotherapy. Aliment Pharmacol Ther. 2013 Jun;37(11):1046–56.
- White ID, Wilson J, Aslet P, Baxter AB, Birtle A, Challacombe B, et al. Development of UK guidance on the management of erectile dysfunction resulting from radical radiotherapy and androgen deprivation therapy for prostate cancer. Int J Clin Pract. 2015 Jan;69(1):106–23.
- Yiannopoulou KG, Anastasiou AI, Kontoangelos K, Papageorgiou C, Anastasiou IP. Cognitive and Psychological Impacts of Different Treatment Options for Prostate Cancer: A Critical Analysis. Curr Urol. 2020 Dec;14(4):169–77.
- Zhao J, Zhu S, Sun L, Meng F, Zhao L, Zhao Y, et al. Androgen Deprivation Therapy for Prostate Cancer Is Associated with Cardiovascular Morbidity and Mortality: A Meta-Analysis of Population-Based Observational Studies. Kyprianou N, editor. PLoS ONE. 2014 Sep 29;9(9):e107516.
This publication has been reviewed for accuracy and updated by:
- Professor Francis Chinegwundoh MBE, Consultant Urological Surgeon, Barts Health NHS Trust, London
- Richard Gledhill, Prostate Cancer Nurse Specialist, Queen Elizabeth Hospital, Birmingham
- Maggie Bingle, Prostate Cancer Clinical Nurse Specialist, East Suffolk and North Essex NHS Foundation Trust
- Our Health Information team
- Our Specialist Nurses.

