Using artificial intelligence to spot aggressive prostate cancer
What you need to know
- Professor Peter Gardner and Dr Ashwin Sachdeva are researching a way to identify low or intermediate risk prostate cancers that might turn into more aggressive disease.
- They will use a special infrared camera to take pictures of prostate tissue and special software using artificial intelligence to analyse these pictures.
- They hope that this research will help doctors know which men with prostate cancer need treatment and which can be safely observed.
What will Professor Gardner, Dr Sachdeva and their teams do?
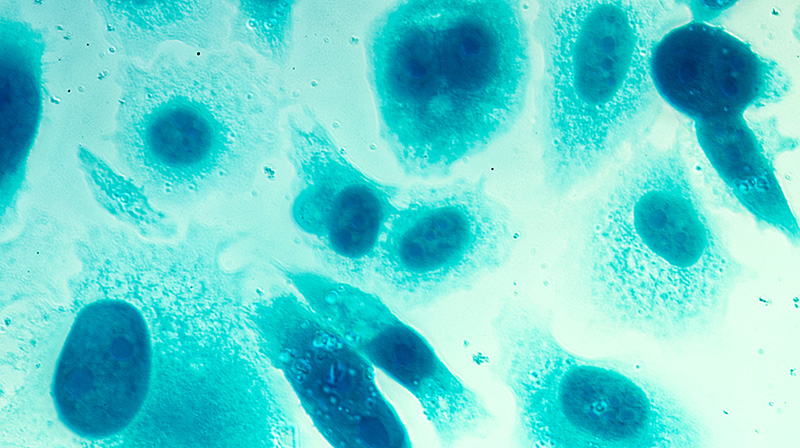
If a man has suspected prostate cancer, he will usually be sent for a biopsy, where small samples of his prostate are taken for testing. These are cut into thin sections, placed on glass slides, and stained using dyes.
A trained pathologist then examines these samples under a microscope, focusing on the arrangement and appearance of the cells to determine whether the man has prostate cancer.
If the man does have prostate cancer, these features can also help estimate the aggressiveness of the disease. Men with ‘low risk’ prostate cancer can often be monitored safely without treatment (active surveillance), while men with ‘high risk’ cancer may need to be moved onto treatment right away.
However, this analysis can be subjective, particularly when the cancer does not have obvious features of ‘high risk’ or ‘low risk’ disease. This means that different pathologists may come to slightly different conclusions on how aggressive the cancer is, which may determine whether the cancer can be safely monitored or whether immediate treatment would be more beneficial for the patient.
The team hopes to develop a technique that can reduce this uncertainty, by gathering more information about the make-up of the prostate cells and using artificial intelligence to interpret the data.
The team will use a special camera called an infrared hyperspectral imaging camera to take pictures of prostate cells from men’s biopsies. This camera takes pictures using infrared light, and can identify changes in the chemistry of prostate cells by analysing how the cells absorb or reflect light.
The researchers will then use these pictures to create a computer model that can predict which prostate cancers are likely to be more aggressive. To do this, they will use a type of artificial intelligence (called machine learning) to train the model to recognise which patterns in the pictures tend to appear in the most aggressive cancers.
They will test the accuracy of his computer model by comparing its predictions with data from a group of men who have already been diagnosed with prostate cancer and followed up over time.
How will this benefit men?
If this research is successful, it could lead to better treatment for men with prostate cancer. Currently, doctors rely on a combination of physical exams, blood tests, MRI scans, and biopsies to diagnose and treat prostate cancer. These methods are not always accurate, and some men with low-risk prostate cancers may be treated unnecessarily. On the other hand, some men with high-risk prostate cancers may not get the treatment they need.
This research could help doctors make more accurate predictions about which men with prostate cancer are at high risk and which are at low risk. This could lead to more personalized treatment plans for men with prostate cancer. For example, men with low-risk prostate cancers might be able to avoid unnecessary treatments and side effects, while men with high-risk prostate cancers might be able to get the treatment they need sooner.
Overall, the research could help improve the lives of men with prostate cancer by helping them get the right treatment at the right time.
Grant information
Reference: RIA21-ST2-011
Researcher: Professor Peter Gardner and Dr Ashwin Sachdeva
Institution: University of Manchester
Award: £117,580
Help us fund more research like this
Your donation helps us fund lifesaving research into better treatments for prostate cancer.