What do my test results mean?
Your doctor will look at your test results, such as your prostate biopsy and scan results, to find out if the cancer has spread (its stage) and how quickly it might be growing.
Watch our animation about understanding your prostate cancer below:
Prostate biopsy results
Your prostate biopsy results will show if any cancer was found and how aggressive it is (how likely it is to spread outside the prostate). You might hear this called your Gleason grade, Gleason score or grade group.
Gleason grade
Prostate cells seen under the microscope have different patterns, depending on how quickly they’re likely to grow. The pattern is given a grade from 1 to 5 – this is called the Gleason grade. If you have prostate cancer, you will have Gleason grades of 3, 4 or 5. The higher the grade, the more likely the cancer is to grow and spread outside the prostate.
Gleason score
There may be more than one grade of cancer in the biopsy samples. Your Gleason score is worked out by adding together two Gleason grades.
Gleason score = the most common grade + the highest other grade in the samples
For example, if the biopsy samples show that:
- most of the cancer seen is grade 3, and
- the highest grade of any other cancer seen is grade 4, then
- the Gleason score will be 7 (3+4).
If your Gleason score is made up of two of the same Gleason grades, such as 3+3, this means that no other Gleason grade was seen in the samples.
If you have prostate cancer, your Gleason score will be between 6 (3+3) and 10 (5+5).
Grade group
Your doctor might also talk about your "grade group". This is a newer system for showing how aggressive your prostate cancer is likely to be. Your grade group will be a number between 1 and 5 (see below).
What does the Gleason score or grade group mean?
The higher your Gleason score or grade group, the more aggressive the cancer and the more likely it is to grow and spread. We've explained the different Gleason scores and grade groups that can be given after a prostate biopsy below. This is just a guide. Your doctor or nurse will talk you through what your results mean.
Gleason score 6 (3 + 3)
All of the cancer cells found in the biopsy look likely to grow very slowly, if at all (grade group 1).
Gleason score 7 (3 + 4)
Most of the cancer cells found in the biopsy look likely to grow very slowly. There are some cancer cells that look likely to grow at a moderately quick rate (grade group 2).
Gleason score 7 (4 + 3)
Most of the cancer cells found in the biopsy look likely to grow at a moderately quick rate. There are some cancer cells that look likely to grow very slowly (grade group 3).
Gleason score 8 (3 + 5)
Most of the cancer cells found in the biopsy look likely to grow slowly. There are some cancer cells that look likely to grow quickly (grade group 4).
Gleason score 8 (4 + 4)
All of the cancer cells found in the biopsy look likely to grow at a moderately quick rate (grade group 4).
Gleason score 8 (5 + 3)
Most of the cancer cells found in the biopsy look likely to grow quickly. There are some cancer cells that look likely to grow very slowly (grade group 4).
Gleason score 9 (4 + 5)
Most of the cancer cells found in the biopsy look likely to grow at a moderately quick rate. There are some cancer cells that are likely to grow quickly (grade group 5).
Gleason score 9 (5 + 4)
Most of the cancer cells found in the biopsy look likely to grow quickly. There are some cancer cells that look likely to grow at a moderately quick rate (grade group 5).
Gleason score 10 (5 + 5)
All of the cancer cells found in the biopsy look likely to grow quickly (grade group 5).
Read more about prostate biopsy results.
What stage is my cancer?
The stage of your cancer tells you whether it has spread outside the prostate and how far it has spread. You might need scans, such as an MRI, CT or bone scan, to find out the stage of your cancer.
A common way to record the stage of your cancer is the TNM (Tumour-Nodes-Metastases) system.
T stage
The T stage shows how far the cancer has spread in and around the prostate. An MRI scan or digital rectal examination (DRE) is usually used to find out the T stage, and sometimes a CT scan.
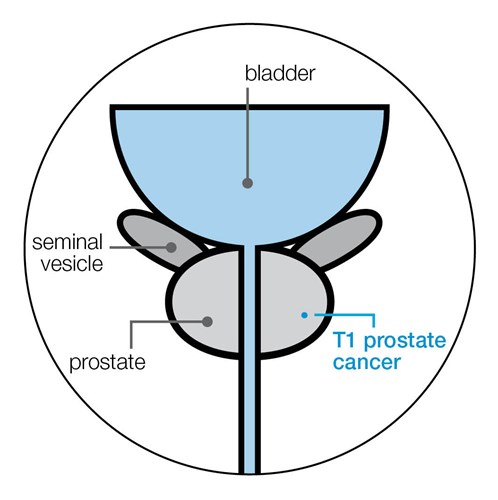
T1 prostate cancer
The cancer can't be felt during a DRE or seen on scans, and can only be seen by looking at your biopsy sample under a microscope.
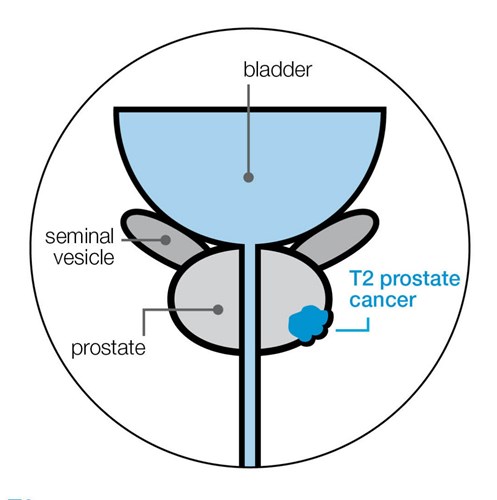
T2 prostate cancer
The cancer can be felt during a DRE or seen on scans, but is still contained inside the prostate.
- T2a The cancer is in half of one side (lobe) of the prostate, or less.
- T2b The cancer is in more than half of one of the lobes, but not in both lobes of the prostate.
- T2c The cancer is in both lobes but is still inside the prostate.
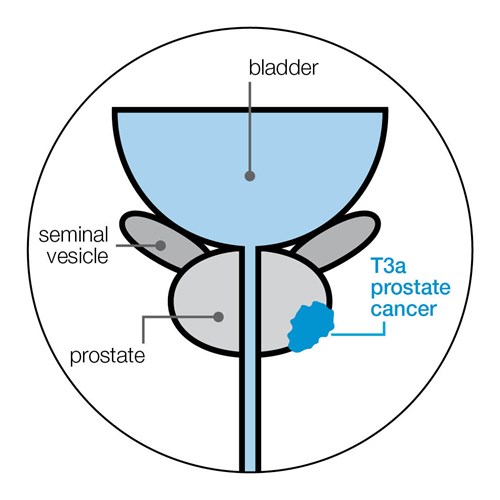
T3 prostate cancer
The cancer can be felt during a DRE or seen breaking through the outer layer (capsule) of the prostate.
- T3a The cancer has broken through the outer layer of the prostate, but has not spread to the seminal vesicles (which produce and store some of the fluid in semen).
- T3b The cancer has spread to the seminal vesicles.
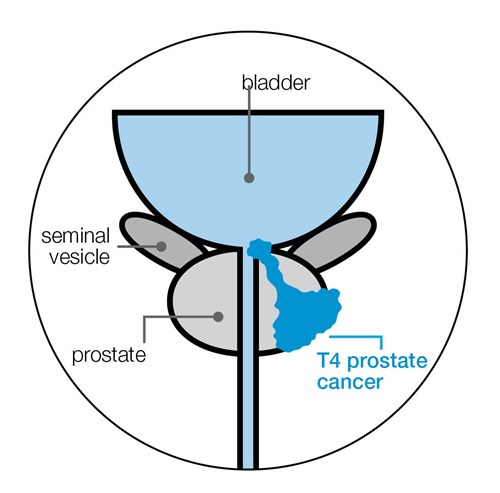
T4 prostate cancer
The cancer has spread to nearby organs, such as the bladder, back passage or pelvic wall.
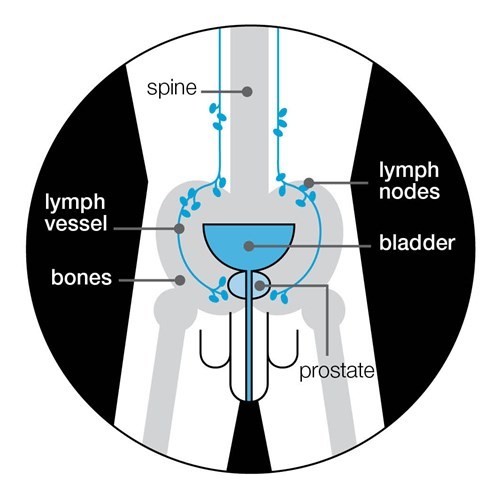
N stage
The N stage shows whether the cancer has spread to the lymph nodes near the prostate. Lymph nodes are part of your immune system and are found throughout your body. The lymph nodes near your prostate are a common place for prostate cancer to spread to.
An MRI or CT scan is used to find out your N stage.
The possible N stages are:
- NX The lymph nodes were not looked at, or the scans were unclear.
- N0 No cancer can be seen in the lymph nodes.
- N1 The lymph nodes contain cancer.
If your scans suggest that your cancer has spread to the lymph nodes (N1), you will be diagnosed with either locally advanced or advanced prostate cancer. This will depend on whether the cancer has spread to other parts of the body.
M stage
The M stage shows whether the cancer has spread (metastasised) to other parts of the body, such as the bones. A bone scan or MRI is usually used to find out your M stage.
The possible M stages are:
- MX The spread of the cancer wasn’t looked at, or the scans were unclear.
- M0 The cancer hasn’t spread to other parts of the body.
- M1 The cancer has spread to other parts of the body.
If you have a scan and it shows your cancer has spread to other parts of your body (M1), you will be diagnosed with advanced prostate cancer.
M1 is split into M1a, M1b and M1c:
- M1a means the cancer has spread to lymph nodes outside of the pelvis
- M1b means the cancer has spread to the bone
- M1c means the cancer has spread to other parts of the body such as the liver or lungs.
What does my TNM stage mean?
Your TNM stage is used to work out if your prostate cancer is localised, locally advanced or advanced. This can help you doctor see how far it has spread and which treatment might be suitable for you.
Localised prostate cancer
Cancer that's contained inside the prostate. Sometimes called early prostate cancer.
Possible TNM stages are:
• T stage: T1 or T2
• N stage: N0 or NX
• M stage: M0 or MX.
Locally advanced prostate cancer
Cancer that’s started to break out of the prostate or has spread to the area just outside it.
Possible TNM stages are:
• T stage: T1 or T2
• N stage: N1
• M stage: M0
or
• T stage: T3 or T4
• N stage: N0 or N1
• M stage: M0.
Advanced prostate cancer
Cancer that’s spread from the prostate to other parts of the body. Also known as metastatic prostate cancer.
Possible TNM stages are:
• T stage: any T stage
• N stage: any N stage
• M stage: M1.
Cambridge Prognostic Group (CPG)
If you have localised or locally advanced prostate cancer, your doctor may talk to you about the risk of your cancer spreading outside the prostate. To work out your risk, your doctor will look at your PSA level, your Gleason score (or grade group) and the T stage of your cancer.
These three factors will place you in one of five categories that form the Cambridge Prognostic Group (CPG). This system is used to help your doctor decide which treatment options are suitable to you, based on your risk.
The CPG system does not apply if you have advanced prostate cancer (cancer that’s spread from the prostate to other parts of the body).
The five CPG categories are described below. If you have any questions about your CPG speak to your doctor or specialist nurse.
CPG 1
- Gleason score 6 (grade group 1), and
- PSA less than 10 ng/ml, and
- T stage of 1 or 2.
This means your cancer is likely to grow very slowly and very unlikely to spread. Your treatment options may include active surveillance, surgery and radiotherapy.
CPG 2
You will be in this group if you have a T stage of 1 or 2 and one of the following:
- Gleason score is 3 + 4 = 7 (grade group 2), or
- PSA 10 to 20 ng/ml.
This means your cancer is likely to grow slowly and unlikely to spread. Your treatment options may include active surveillance, surgery or radiotherapy with hormone therapy.
CPG 3
- Gleason score 3 + 4 = 7 (grade group 2), and
- PSA 10 to 20 ng/ml, and
- T stage of 1 or 2.
You will also be in this group if you have:
- Gleason 4 + 3 = 7 (grade group 3), and
- T stage of 1 or 2.
This means there is a medium (intermediate) risk of your cancer growing and spreading out of your prostate. Your treatment options may include surgery or radiotherapy with hormone therapy.
You may also have active surveillance if you don’t want treatment straight away or can’t have treatment.
CPG 4
You will be in this group if you have only one of the following:
- Gleason score 8 (grade group 4), or
- PSA more than 20 ng/ml, or
- T stage 3.
This means that there is a high risk of your cancer growing quickly and spreading out of your prostate. Treatment options may include surgery or radiotherapy with hormone therapy.
CPG 5
You will be in this group if you have two or more of the following:
- Gleason score 8 (grade group 4), and
- PSA more than 20 ng/ml, and
- T stage 3.
You will also be in this group if you have one of the following:
- Gleason score 9 to 10 (grade group 5), or
- T stage 4.
This means that there is a high risk of your cancer growing quickly and it’s very likely to spread. Treatment options may include surgery or radiotherapy with hormone therapy.
Low, medium or high risk prostate cancer
When talking to your doctor about the risk of your cancer spreading, they may refer to low, medium or high risk. This older system also used your PSA level, Gleason score and the T stage of your cancer. You should ask your doctor about your CPG category and what this means in terms of your treatment options.
If you’re concerned that your doctor is using the old system, rather than the CPG system, please talk to them about it. The information on this page can help to inform them of the new system. It's important to remember that both systems are only intended as guides for your doctor, and they will consider many other clinical factors when advising you about your treatment options.
What happens next?
The results should help you and your doctor decide which treatments might be suitable for you. Ask your doctor or nurse to explain your test results if you don’t understand them. Or you could call our Specialist Nurses.
Dealing with prostate cancer
Being diagnosed and living with prostate cancer can change how you feel about life. If you or your loved one is dealing with prostate cancer you may feel scared, stressed or even angry. There is no ‘right’ way to feel and everyone reacts differently.
Visit our wellbeing hub for information to help support you in looking after your emotional, mental, and physical wellbeing. If you are close to someone with prostate cancer, find out more about how you can support someone with prostate cancer and where to get more information.
References
Updated: August 2023|To be reviewed: August 2026
- Peter Hoskin, Consultant Clinical Oncologist, Mount Vernon Cancer Centre and Professor of Clinical Oncology, Division of Cancer Sciences, University of Manchester
- Alissa Lewis, Uro-oncology Clinical Nurse Specialist, Bradford Teaching Hospitals NHS Foundation Trust
- Alastair Thomson, Consultant Clinical Oncologist, Royal Cornwall Hospitals NHS Trust
- Our Specialist Nurses
- Our Volunteers.
- Berney DM. The case for modifying the Gleason grading system. BJU Int. 2007;100(4):725–6
- Epstein JI, Allsbrook Jr WC, Amin MB, Egevad LL, Committee IG, others. The 2005 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol. 2005;29(9):1228–42.
- Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, et al. The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol. 2016;40(2):244–52.
- Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. 22
- Mottet N, Cornford P, van der Bergh RCN, Briers E, Eberli D, De Meerleer G, et al. EAU - EANM - ESTRO - ESUR - ISUP - SIOG Guidelines on Prostate Cancer [Internet]. European Association of Urology; 2023 [cited 2023 Mar 30]. Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-EANM-ESTRO-ESUR-ISUP-SIOG-Guidelines-on-Prostate-Cancer-2023_2023-03-27-131655_pdvy.pdf16
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management [Internet]. 2021 [cited 2022 Dec 19]. Available from: https://www.nice.org.uk/guidance/ng131

