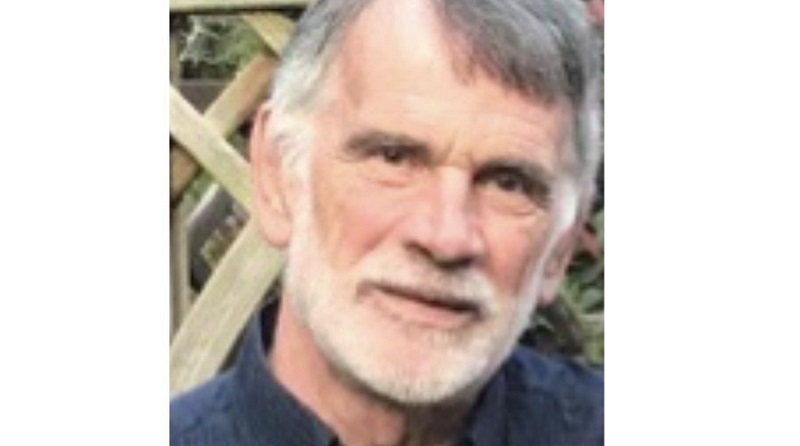
Charlie's Story
Charlie, 66, was diagnosed with prostate cancer in 2020. He had surgery to remove his prostate. Here, he talks through his experience.
My diagnosis experience
My father experienced prostate problems in his later years. Looking back, he may have had prostate cancer, although he didn’t have a formal diagnosis. I didn’t experience any prostate problems until 2019, when I had a quite severe urinary tract infection (UTI). It took two courses of antibiotics to clear the infection, so my GP did a digital rectal examination (DRE). My DRE was fine, but I had a PSA blood test which showed a PSA level of 18. This was high but not unusual when you have a UTI. Because the doctor was unsure why I had the UTI and why it was being difficult to get rid of, he decided to refer me to the urology department at the hospital.
I had tests which looked at urine retention and urine flow, and another DRE. The DRE didn’t pick up anything unusual. However, the urine retention test did show that I was retaining some urine when trying to empty my bladder. The doctor gave me a course of tamsulosin, a common medicine for helping urine flow, which did seem to help. I wasn't waking up at night to urinate or anything. I did have a weaker flow and found myself needing to go more frequently. But I didn't, at the time, recognise that these may have been signs and symptoms. I just put it down to getting older.
Following on, I had a follow up PSA blood test 3 months later, which was 5.7. And another one 6 months later, which was 3.7. The doctor told me they were high but ‘normal’ for me. But they decided to monitor my PSA levels and suggested doing an MRI to get a baseline. After the MRI, they also suggested that I should have a template transperineal biopsy under sedation.
After the biopsy, I got a call from the consultant with the results of the biopsy; there was cancer in both sides of the prostate and it looks like it’s contained within the prostate. My reaction to this was both thankfulness and relief – thankful that my prostate cancer had been diagnosed at an early, contained stage and relief that there were treatment options that seemed to offer a ‘complete’ cure.
Deciding a treatment
They discussed my treatment options which were active surveillance, radiotherapy or surgery. The oncologist talked to me about the non-surgical options, but they didn’t appeal to me to be honest. I wasn’t keen on the idea of active surveillance because it meant I may need regular biopsies. I also felt that there were two other options (surgery and radiotherapy) that seemed to offer a more permanent solution.
The key points that helped me decide to have surgery (radical prostatectomy) over radiotherapy were that, if radiotherapy didn’t work, it could make surgery more difficult in the future. I also found the idea of hormone therapy and weeks of daily appointments for radiotherapy fairly daunting. So, I pretty much made my mind up at the point and decided surgery was the right option for me.
Over the next couple of weeks, I had conversations with nurses and doctors at the hospital and talked through my questions about incontinence. I was more concerned with incontinence after surgery than the sexual side effects, as I already had a history of some erectile dysfunction. My consultant informed me that surgery would not improve this. As trivial as it may seem, I wanted to get back to riding my bike again. The doctors and nurses were able to answer all my questions on recovery time which was reassuring.
Treatment experience
The surgery itself and recovery was fine, the surgeon said it all went well and I was sent home the following day. I left hospital with a catheter, and had it removed after a week. I wore men’s incontinence pads for a period of time. I also received a surgery support pack from Prostate Cancer UK which included a variety of pads which was really helpful. I was pretty much dry after 4 weeks which was really quick. Incontinence was the main fear for me before surgery, so I was very happy about that.
One thing I wished I discussed more before the surgery was nerve sparing. I wished I asked more question as I got the impression that in my case it wasn’t possible and had non-nerve sparing surgery.
Life after surgery
It has been 3 years since my operation. I had a follow up PSA blood test every three months for the first year and every 6 months in the second year. My PSA blood tests have all come back with a PSA level of less than 0.01 or non-detectable.
It might seem strange, that I see my prostate cancer as an event in my life that happened and now is over. Although, I will have my PSA level monitored for at least 5 years, and I still have still have some issues, on occasion suffer from stress incontinence, if I’m not careful about getting up off a seat. But I still do my pelvic floor exercises, which I don’t find easy to do but they help a lot.
I am now back riding my bike, 30 to 50 miles a week, which had been really enjoyable
Updated September 2023


