Can 'direct from patient' samples be used to test promising new treatments for prostate cancer?

Grant information
Institution – University College London
Researchers – Dr Susan Heavey
Grant award - £309,792
Duration of funding – 2018-2023
Status - Complete
Reference – TLD-PF16-004
We will improve the success rate of drug development be testing treatments on a wide range of cell types and looking at the effects of these treatments on thousands of genes.
Why did we fund this project?
- No two prostate cancers are the same and can have very different responses to the same treatment. Personalising drug development could help men receive the most beneficial drug for them.
- Dr Heavey wanted to develop improved ways to test new treatment ideas and to find out which men are most likely to benefit from which treatment.

- She hoped that using ‘direct from patient’ prostate cancer samples - rather than animal models or cancer cells grown in a dish - would be an effective approach.
- We also wanted to support Dr Heavey in establishing her own research team dedicated to developing better drug testing methods and tailoring treatments to individual men.
What did the team do?
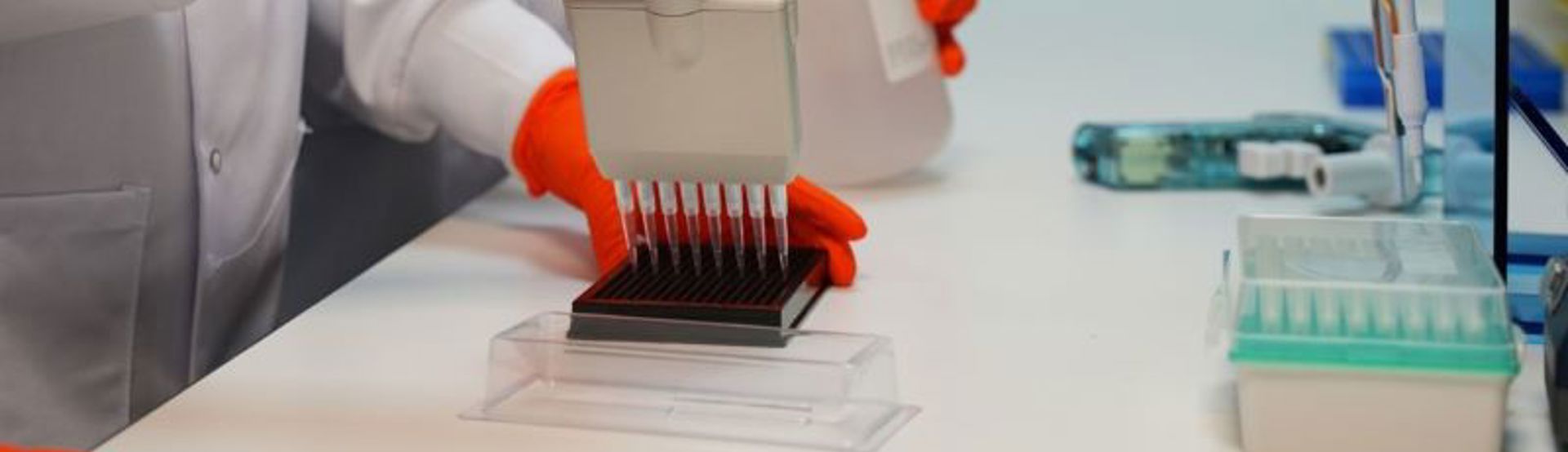
- The team developed new methods to create patient-derived explants from tiny slices of prostate cancer donated by men during surgery to remove their prostate.
- These explants contain dozens of different cell types arranged in complex structures found in the body, providing a more realistic model of prostate cancer compared to traditional cell lines, which often consist of single cell types grown in uniform layers in a plastic culture dish.
- By including the surrounding healthy cells, the explants also better reflect the natural cancer environment, which can influence how the cancer grows, drug responses and interactions with the immune system.
What did the team achieve?
- The team produced a collection of patient-derived explants that preserve the diverse range of cell types and structures found in and around prostate cancer in the body.
- Remarkably, the activity of thousands of genes can be monitored across these various cell types and structures. This will help researchers understand the potential effects of new treatments for each man and better predict whether a drug can kill cancer cells without harming healthy cells.

- Two new drug treatments were tested using the explants, suggesting promising benefits for some men, and demonstrating the value of identifying those who are not likely to respond to new therapies before proceeding to clinical trials.
- Dr Heavey has established herself as an expert in her field, successfully leading a thriving research team with independent funding to further advance her important work.
What does this mean for men?
- Improving drug development to find out which treatments work best for each man will help them choose the most effective treatments and avoid unnecessary side effects.
- Excitingly, Dr Heavey’s team are using the methods they have developed in new research to develop treatments for men whose cancer has stopped responding to radiotherapy, bringing hope for more effective, personalised therapies in the future.
Help us fund more lifesaving research like this...
Your support helps us fund pioneering research, so we can work towards a future where men's lives aren't limited by prostate cancer.

