Reprogramming immune cells to fight prostate cancer

Grant information
Reference: TLD-CAF24-007
Researcher: Dr Ahmet Hazini
Institution: University of Oxford
Award: £340,594
What you need to know
- This project aims to create a new treatment for prostate cancer by changing a man’s own immune cells to better detect and destroy cancer cells.
- The modified cells would act like a vaccine, teaching the immune system to recognise and fight cancer, reducing the risk of the cancer coming back.
- This approach could potentially lead to treatments that work for other types of cancer too, offering new hope for even more people.
About Dr Ahmet Hazini
Dr Hazini completed his master’s degree in biochemistry at Yildiz Technical University, Turkey, before moving to the Technische Universität Berlin (Technical University of Berlin), Germany, to undertake a PhD.
His PhD research focused on using viruses – either genetically engineered or naturally occurring – to selectively target and eliminate tumour cells. This is known as oncolytic virotherapy. After earning his PhD, he continued researching the viruses' immune effects, resulting in several publications and patents.
He then joined Professor Len Seymour's lab at Oxford, where he will be based for this project. During this time, Dr Hazini became interested in the role of immune cells in cancers like prostate cancer. Macrophages, the focus of this project, can get deeper into the area around the tumour than many other immune cells, so he began working on a way to make them active against the disease.
This grant will enable Dr Hazini to take this promising research further as an independent researcher.
Why are we funding this research?
Although early-stage prostate cancer can often be treated effectively, some men will find that their disease comes back, and doesn’t respond as well to treatment. This leaves these men with limited treatment options, and they may find that those treatments that do work can have side effects that impair their quality of life.
Dr Hazini’s research aims to tackle these issues by developing a new, personalised treatment that uses a man’s own immune cells to fight the cancer.
As an added benefit, these modified cells could act like a vaccine, teaching the immune system to recognise and attack cancer cells, reducing the risk of the disease coming back.
This funding will be invaluable in advancing my research and career, enabling the development of cutting-edge, personalised immune therapy for prostate cancer. Through this fellowship, I have the privilege of collaborating with world-leading scientists in prostate cancer and immunotherapy. My goal is to develop innovative prostate cancer vaccines, which could provide an effective treatment option for prostate cancer patients at every stage of the disease.
What will Dr Hazini do?
He will start by collecting immune cells called macrophages from blood samples donated by men with prostate cancer.
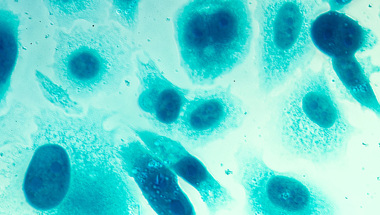
Macrophages are a type of white blood cell that play a crucial role in the body's defence against infections and diseases. However, in men with prostate cancer, these cells often fail to recognise and attack cancer cells effectively. In many cases, the cells support the tumour’s growth instead.
To overcome this, Dr Hazini will modify these macrophages in the lab to enhance their ability to recognise prostate cancer cells as a threat. He will also enable the macrophages to teach other immune cells to recognise the cancer, encouraging the immune system to kill cancer cells when it finds them – for example if the cancer comes back after treatment.
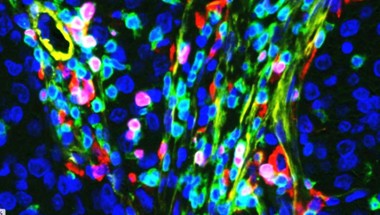
Once the macrophages are modified, Dr Hazini will test them on cancer cells in a flat dish, and then on tumours grown in the lab from prostate cancer samples donated by men with the disease. Compared to traditional cells in a dish, these lab-grown tumours (known as organoids) more closely resemble how cancer grows inside the body, so will give Dr Hazini a better idea of how effective the modified macrophages are likely to be in a person with prostate cancer.
Finally, Dr Hazini will test the macrophages in mice to see how safe and effective the treatment might be in the body.
During the project, Dr Hazini will work closely with Professor Wytske van Weerden at Erasmus University Medical Center in the Netherlands. Professor van Weerden and her team are experts in developing organoids, using them to understand how prostate cancer develops, how it becomes resistant to treatment, and how it could be targeted with new treatments.
How will this benefit men?
This research could lead to a new, highly targeted treatment option that is both more effective and less invasive than existing one-size-fits-all therapies for men with prostate cancer.
Immunotherapy, where the body’s own immune system is encouraged to kill cancer cells, has had limited success in prostate cancer so far. Dr Hazini’s work could therefore open up a new avenue for treating the disease, offering hope and a longer life to men who would otherwise have few treatment options left.
Meanwhile, a treatment using a man’s own immune cells should reduce the risk of side effects typically associated with conventional treatments like chemotherapy and radiation.
If the treatment is also able to reduce the risk of prostate cancer coming back, that could save even more lives, and lessen the anxiety that men face wondering if their cancer will return.
More broadly, the success of this research could pave the way for similar treatments for other types of cancer, broadening its impact and offering hope to many more people.
Help us fund more research like this
Your donation helps us fund lifesaving research that's improving the way we diagnose prostate cancer.