Retraining immune cells to kill prostate cancer

Grant information
Reference: TLD-CAF24-006
Researcher: Dr Koichi Sasaki
Institution: Imperial College London
Award: £347,846
What you need to know
-
This project will look at a potential new treatment that targets and kills prostate cancer cells using modified versions of the body's own immune cells.
-
The cells release a ‘homing beacon’ when they reach the tumour, boosting the immune system’s response against the disease and helping other immune cells attack the cancer.
-
The research will test the therapy's safety and effectiveness in advanced prostate cancer, to gather evidence for the treatment to be tested by men in future.
About Dr Koichi Sasaki
Dr Sasaki completed his master’s degree in materials science and engineering at Kyushu University, Japan, before starting a PhD in engineering at the same institution.
During his PhD, Dr Sasaki also spent nine months at the University of Chicago, USA, as a visiting student, learning about cancer immunotherapy.
After completing his PhD in 2020, he took on a postdoctoral fellowship at Osaka Prefecture University, Japan, before moving to the lab of Dr Jun Ishihara at Imperial College London to work on T cell immunotherapy. This was a departure from the usual research being done by Dr Ishihara’s team, but it led to the cells that form the basis of this research project.
This grant will enable Dr Sasaki to take this promising research further as an independent researcher.
Why are we funding this research?
Immunotherapy – using the body’s immune system to fight off cancer – has revolutionised the way we treat some cancers but, so far, it's had limited success in prostate cancer. This project aims to change that.
That would be a big benefit to men – especially as the kind of immunotherapy Dr Sasaki is researching has been particularly effective, putting 75 to 95 per cent of some blood cancers into remission. But it’s not yet been possible to use it to treat cancers that form solid tumours, like prostate cancer.
This is because of two main challenges. The first is getting the immune cells into the tumour and making sure that they stay there. And the second is ensuring that the immune cells only attack cancer cells, and not other, healthy cells that the body still needs.
This research project will look for ways to solve these problems, meaning it could open up a new type of treatment to men with prostate cancer.
It is my great pleasure to receive Fellowship funding from Prostate Cancer UK. This provides me the independence and opportunity to be skilled in advanced preclinical prostate cancer models through collaboration with outstanding investigators. Using the models, I will test the safety and therapeutic effect of innovative immune cell therapy. One day, that may turn into a new treatment to benefit men with currently incurable prostate cancer.
What will Dr Sasaki do?
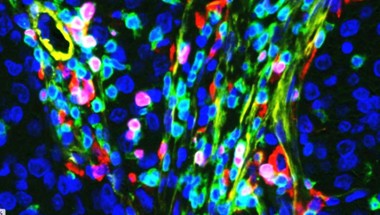
Working with Dr Jun Ishihara, also at Imperial College London, Dr Sasaki has created mouse immune cells that release a ‘homing beacon’ when they come across prostate cancer.
This homing beacon (called IL-12) draws other immune cells to the area, to encourage them to kill the cancer - an approach that's already shown promise in a clinical trial of a treatment for melanoma.
However, the trial also found that the IL-12 ended up spreading around the body, which can lead to severe side effects.
That’s why Dr Sasaki has tweaked the IL-12 in his cells to stick to a molecule called collagen. There is a lot of collagen in and around prostate cancer tumours, meaning this tweak should help the IL-12 stay in the area around the cancer cells.
The first step in this project will be to test that these modified immune cells are safe and effective in mice.
If so, Dr Sasaki will then create the same thing using human immune cells, and check that they work in the same way. For example, can they be grown as easily, can they still detect prostate cancer cells, and can they still release IL-12 when they do?
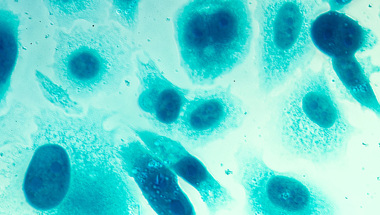
After these checks, Dr Sasaki test the cells on mini tumours (known as organoids), grown from samples of prostate cancer donated by men with prostate cancer. Unlike cells grown flat in a dish, these organoids are 3D, so they’re a good test for how the immune cells will respond to an actual tumour in the body.
Finally, Dr Sasaki will implant these prostate cancer samples into mice, and give them the modified immune cells, to see how safe and effective they are in the body.
During the project, Dr Sasaki will work closely with Professor Johann de Bono at The Institute of Cancer Research, London. Professor de Bono and his team are experts in developing organoids and using them to test the effectiveness of new treatments.
How will this benefit men?
Dr Sasaki's research could lead to a new, more targeted and effective treatment for men. Traditional treatments, such as chemotherapy and radiotherapy, can damage cancer cells and healthy cells alike, leading to side effects. Dr Sasaki's approach uses immune cells that specifically target prostate cancer cells, reducing the risk of harm to healthy cells.
These immune cells also deliver drugs directly to the tumour, enhancing the treatment's effectiveness and attracting other immune cells to join the fight. This method could help to both kill the existing cancer and, potentially, provide lasting protection by teaching the immune system to recognise and kill future cancer cells, reducing the risk of the disease coming back.
If successful, this could transform the way we treat the disease, helping more men survive prostate cancer while minimising the side effects they experience.
Help us fund more research like this
Your donation helps us fund lifesaving research that's improving the way we treat prostate cancer.