Unlocking personalised medicine in advanced prostate cancer

Grant information
Reference: TLD-CAF24-001
Researcher: Dr Emma Lishman-Walker
Institution: Newcastle University
Award: £347,412
What you need to know
-
Hormone therapies like enzalutamide help a lot of men, but sometimes prostate cancer will keep growing despite the treatment.
-
A type of treatment called a kinase inhibitor may help in these cases, but it’s not always clear in advance which men will benefit.
-
Dr Lishman-Walker aims to develop a test that can spot which men will benefit from kinase inhibitors, without the need for a biopsy.
-
This could help to personalise treatment for men with prostate cancer, ensuring each man gets the most effective therapy for him, with fewer side effects.
About Dr Emma Lishman-Walker
Dr Lishman-Walker completed a master’s degree in biosciences, followed by a PhD, at Newcastle University.
During her PhD, Dr Lishman-Walker worked in a team studying childhood brain tumours and looked for ways to categorise and understand the development of these cancers, as part of work to find new ways to treat them.
Since finishing her PhD in 2021, she has been working as a research associate in Dr Kelly Coffey’s lab at Newcastle University, working in prostate cancer research while working to publish the findings from her PhD.
In that time, Dr Lishman-Walker has been working on further advancing our understanding of how prostate cancer responds to kinase inhibitors. This grant will enable her to extend this promising research as an independent researcher.
Why are we funding this research?
This project will help to tackle one of the biggest challenges in prostate cancer: what to do when treatments stop working (known as treatment resistance).
Prostate cancer often relies on testosterone to grow, and treatments like enzalutamide work by reducing testosterone levels in the body. However, sometimes prostate cancer can find a way to keep growing even when testosterone is low, making these treatments less effective over time.
Dr Lishman-Walker and her colleagues have previously found that a set of molecules in the body called kinases can help prostate cancer grow even when testosterone levels are low.
This project will build on that work, by developing a test that can spot which men are most likely to benefit from treatments to stop these kinases from working (called kinase inhibitors).
That’s vital because it’s not always clear from the outset which men will actually benefit from kinase inhibitors. This makes it difficult for researchers to collect enough evidence to get them approved as a treatment for the disease.
A test to predict which men will benefit from kinase inhibitors would therefore help to speed up their approval as a treatment for prostate cancer, and would also give doctors more confidence in prescribing them.
This Prostate Cancer UK Career Acceleration Fellowship will be key in helping me to establish my own research to develop a blood test to predict which men might benefit from personalised kinase inhibitor treatment, reducing the need for invasive prostate cancer biopsy.
What will Dr Emma Lishman-Walker do?
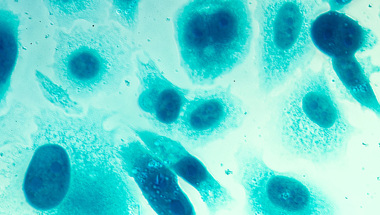
In her project, Dr Lishman-Walker will grow prostate cancer cells in the lab and treat them with a range of kinase inhibitors, either alone or alongside enzalutamide.
Some of the cells will be resistant to enzalutamide and others will not be, to see if there is a difference in how the two types of cells respond. This could give an indication of whether kinase inhibitors are better given to men earlier or later in the course of their treatment.
After treating these cells, Dr Lishman-Walker will study how they react, focusing on which genes become more, or less, active in response to the treatment. How the cells respond to each kinase inhibitor will tell her what a test should look for in men who will – or won’t – respond to them in future.
Ideally this would be something that could be measured in blood or urine samples, to reduce the need for prostate biopsies, making the process easier and more comfortable for men with the disease.
For that reason, Dr Lishman-Walker will work closely with Dr Jason Webber at Swansea University throughout this project, to find a way to detect these clues in blood samples.
She will also test these findings on tumour samples from men with prostate cancer, to improve the chances of the results being consistent between the lab and real-life tumours.
How will this benefit men?
A test to detect which prostate cancers will respond to kinase inhibitors (and, if so, which ones) would make it much easier for these drugs to be trialled as a new treatment for prostate cancer.
If the drugs went on to be approved, such a test would enable doctors to predict which men would benefit from being prescribed kinase inhibitors, and at what stage of their treatment plan.
This means that men with prostate cancer could receive treatments that are much more tailored to their specific cancer type, improving the chances of success and reducing unnecessary side effects.
What's more, a test based on blood or urine samples could make assigning these treatments and monitoring their progress easier and more comfortable for men, by reducing the need for biopsies.
Help us fund more research like this
Your donation helps us fund lifesaving research into better treatments for prostate cancer.