Avoiding unnecessary prostate biopsies by using new MRI techniques (ASPIRE trial)

Grant information
Reference: MA-TIA24-006
Researchers and Institutions:
Professor Shonit Punwani, University College London
Professor Caroline Moore, University College London
Professor David Atkinson, University College London
Associate Professor Eleftheria Panagiotaki, University College London
Associate Professor Iztok Caglic, University College London Hospitals NHS Foundation Trust
Award: £1,481,377
What you need to know
- Every year, thousands of men undergo prostate biopsies after MRI scans, but about half of these biopsies find no serious cancer.
- This project is testing new, more precise MRI scans that could help doctors decide when a biopsy is truly needed, potentially avoiding many unnecessary procedures.
- Researchers will test these scans across different hospitals and MRI machines to prepare for a nationwide clinical trial.
Why are we funding this research?
Right now, if a man has an MRI that could show prostate cancer, the next step is usually a biopsy, where a sample from the prostate is taken to check for cancer. But about half of these biopsies turn out to be unnecessary, finding no serious cancer. That means thousands of men each year go through a painful and sometimes risky procedure they didn’t need.
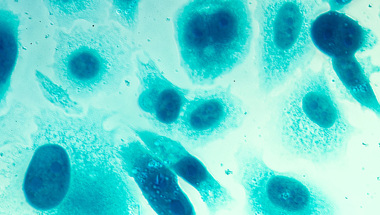
This project is working to change that, building on the team’s earlier work on a new scanning technique called VERDICT, which can be done on existing MRI machines, but give doctors a clearer picture of whether a biopsy is really needed. It will test VERDICT and two other similar techniques to compare them and make sure they work consistently across several types of MRI machines and in different NHS hospitals.
This work will enable them to carry out a later, larger clinical trial that would give us the evidence for or against introducing the scans across the country.
What will the researchers do?
First, they’ll set up the advanced scanning techniques –VERDICT, RSI, and fast VERDICT – on MRI machines from the three main manufacturers used in NHS hospitals (GE, Siemens, and Philips). This is important because different machines can produce slightly different results, and the team needs to make sure the scans work reliably across all of them.
To calibrate the scanners, the researchers will scan around 20 men twice – once at their main hospital and again at a second hospital with a different scanner. This calibration will help ensure that scan results across the trial are comparable, no matter where they’re done.
At the same time, they’ll run a larger study across four hospitals, scanning 600 men who are being checked for prostate cancer. These men will have the new scans added to their usual MRI, but the results won’t be used to make clinical decisions yet. Instead, the researchers will compare how well each scanning method performs in spotting men who truly need a biopsy.
Finally, at one hospital, they’ll test using VERDICT scans to guide biopsy decisions in real time. If the scan suggests no serious cancer, the man may avoid a biopsy, but he’ll be followed up a year later to make sure nothing was missed. This phase will help the team understand how the scan could be used safely in practice and how men feel about avoiding a biopsy.
Together, these steps will lay the groundwork for a future national trial and, potentially, a change in how prostate cancer is diagnosed across the NHS.
A lot of detailed information from MRI can’t be used to make decisions because it varies from scanner to scanner. If we could use this information, we could harness the full power of MRI and make better clinical decisions. This study will work out how to do this across different hospitals, so that only men that have significant disease undergo biopsy.
How will this benefit men?
Currently, many men go through a biopsy after an MRI scan, only to find out they don’t have a serious cancer. Although research has massively reduced the risks that are linked to biopsies, they can still be painful, cause bleeding or infection, and lead to a lot of anxiety.
By improving MRI scans so they give clearer, more detailed information, this project could help doctors decide more accurately who really needs a biopsy and who doesn’t. That means fewer men would go through an unnecessary and uncomfortable procedure, while still making sure that serious cancers are caught early.
For men with low-risk cancers being monitored over time, the new scans could also reduce the need for repeated biopsies.
In the long run, this approach could improve men’s experience of prostate cancer testing, reduce stress and side effects, and help the NHS use its resources more efficiently.
Help us fund more research like this
Your donation helps us fund lifesaving research into better ways to diagnose prostate cancer.