Bisphosphonates for advanced prostate cancer
This page has information about bisphosphonates, which can be used to treat bone problems or prevent further bone damage if your cancer has spread to the bones (advanced prostate cancer).
We explain how bisphosphonates work, what treatment involves, and the advantages and disadvantages of having bisphosphonates for advanced prostate cancer. We also describe the possible side effects of bisphosphonates and ways to manage these.
If you've been diagnosed with localised prostate cancer that hasn't spread outside the prostate, read our information on treatments for localised prostate cancer instead.
What are bisphosphonates?
Bisphosphonates are a type of drug that can help to strengthen bones that have become weak or thin. This may be caused by cancer that has spread (advanced prostate cancer), but can also happen if you’re having hormone therapy. This is because the treatment can change the structure of bones and make them very weak – a condition called osteoporosis.
Bisphosphonates can be given either as tablets or through a drip into a vein in the arm.
Who can have bisphosphonates?
You may be offered bisphosphonates if you have:
- bone thinning (osteoporosis) caused by hormone therapy
- bone weakness caused by prostate cancer that has spread to the bones
- bone pain if other pain-relieving treatments aren’t helping
- hypercalcaemia – a very rare condition in people with prostate cancer, caused by high levels of calcium in the blood.
Bisphosphonates to treat bone thinning (osteoporosis) caused by hormone therapy
Some types of hormone therapy, a common treatment for prostate cancer, can make your bones weaker and cause a condition called osteoporosis. This can increase your risk of broken bones (fractures) and cause bone pain. Bisphosphonates can strengthen bones and prevent further bone thinning.
Bisphosphonates to treat bone weakness caused by prostate cancer that has spread to the bones
If prostate cancer spreads to the bones, the cancer can damage them and cause pain. Bisphosphonates can strengthen the bones and slow down further bone damage. This can help to prevent broken bones and reduce the need for radiotherapy – a treatment to reduce pain when cancer has spread to the bones.
Bisphosphonates for bone pain
Bisphosphonates are sometimes used to help relieve and prevent further bone pain. They are sometimes given at the same time as painkillers, but are usually only used if other pain-relieving treatments aren’t working very well.
Bisphosphonates to help hypercalcaemia
Bisphosphonates can also be used to treat a condition called hypercalcaemia, which is a high level of calcium in the blood. It is very rare, but can sometimes affect men with advanced prostate cancer.
If you live in England, Wales or Northern Ireland, you should be able to have bisphosphonates if your doctor thinks they are suitable for you.
In Scotland, bisphosphonates aren’t widely available for men with prostate cancer. If you live in Scotland, speak to your doctor about whether you can have bisphosphonates.
If you’ve had problems with your kidneys, teeth or jaw in the past, you may not be able to have bisphosphonates. This is because, very rarely, bisphosphates can cause jaw bone problems (osteonecrosis of the jaw). Talk to your doctor or nurse about whether bisphosphonates are suitable for you.
Other treatments that can be used to strengthen the bones include:
-
Surgery to support damaged bone
A metal pin or plate can be inserted into the affected bone to strengthen it and reduce the risk of it breaking. Or, a type of cement can be used to fill the damaged area. This makes the bone stronger and less painful.
-
A drug called denosumab (Xgeva®)
This can help manage bone thinning. It might be an option if bisphosphonates aren’t suitable for you and you live in England, Wales or Scotland. If you live in Northern Ireland, your doctor may be able to apply to your local Health and Social Care (HSC) trust if they think denosumab is suitable for you. This is called an individual funding request.
Other treatments for pain include pain-relieving drugs, pain-relieving radiotherapy, radium-223 (Xofigo®), and surgery to support damaged bone.
If you have hypercalcaemia, other treatments for this include passing fluid through a drip in your arm, to flush calcium out of your blood.
How do bisphosphonates work?
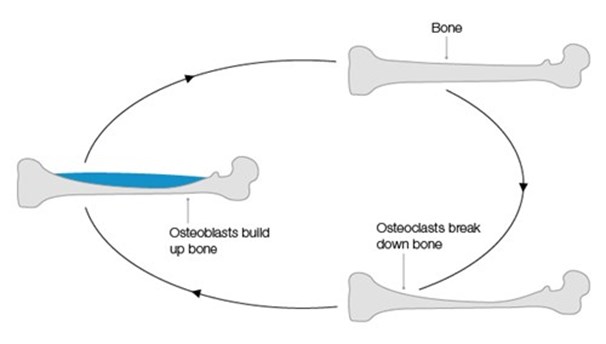
Your bones are made of living tissue and are constantly changing. In healthy bones, cells are always breaking down and rebuilding bone tissue – this is called the bone cycle. There are two types of bone cells that do this job:
- osteoclasts – cells that break down old bone tissue
- osteoblasts – cells that make new bone tissue.
In strong and healthy bones, old bone tissue is broken down at the same rate that new bone tissue is made. But if prostate cancer spreads to the bone, this carefully balanced cycle can change. Two things can happen.
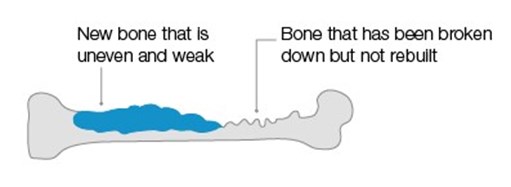
- Bone tissue gets broken down faster than it gets made, so too much bone tissue is destroyed. This can make the bones thinner and weaker. It often happens naturally as men get older and in men who drink lots of alcohol or smoke.
- Bone tissue gets made faster than it gets broken down, so too much bone tissue is made. This is common in men with advanced prostate cancer. When it happens, the bone becomes thicker because of the extra bone tissue. But it is weaker than bone that is made normally, because it doesn’t have chance to become hard or strong.
Both processes can happen at the same time in different areas of the bone. The damage they cause makes the bones weaker, which can increase the risk of broken bones and cause bone pain.
Bisphosphonates can help prevent the breakdown of bone by osteoclasts. They can also help to encourage bone building by osteoblasts. This makes the bone stronger and reduces the risk of broken bones. This might also help to relieve pain, although the evidence for this isn’t very strong.
The bone cycle
This is what happens in normal healthy bone.
Bone damaged by cancer
This is what happens when cancer spreads to the bone.
What are the advantages and disadvantages of bisphosphonates?
As with all drugs, there are advantages and disadvantages of using bisphosphonates. What might be important to one person might not be so important to someone else. If you’re offered bisphosphonates, talk to your doctor or nurse about your own situation – they can help you decide if bisphosphonates are right for you.
Advantages
- Bisphosphonates can make your bones stronger. This may help to reduce your risk of broken bones and other bone problems, such as bone pain.
- Bisphosphonates can delay the need for other treatments for bone problems such as radiotherapy to relieve bone pain or surgery to support damaged bones.
- Bisphosphonates can help to relieve bone pain and stop it getting worse – you may find it easier to move around if you have less bone pain.
- You should still be able to carry on with your normal day-to-day activities, such as driving, while having bisphosphonates.
- Bisphosphonates can lower the amount of calcium in your blood if it’s high (hypercalcaemia), and treat the symptoms.
Disadvantages
- Like all treatments, bisphosphonates can cause side effects.
- If you’re having a bisphosphonate called zoledronic acid (Zometa®) you may have a hospital appointment every three or four weeks for treatment.
- Zoledronic acid is given through a drip (intravenous infusion) into a vein, which can be uncomfortable but shouldn’t be painful.
- If you’re given bisphosphonate tablets, you’ll need to be very careful that you take them correctly.
- If you’re taking bisphosphonates to help with bone pain, they can take up to three months to start helping.
- You may need regular dental check-ups, which some people dislike.
- You’ll need regular blood tests to check your kidneys are working properly.
- You’ll need regular blood tests to check the levels of certain minerals, such as calcium and phosphate, in your blood. If your levels are low, you may need to take supplements.
What does treatment involve?
Before treatment
Before your first treatment, you will have some tests to check your kidneys are working properly. This is because bisphosphonates may affect how well they work. The kidneys get rid of any waste products in your blood, so it’s important to make sure they’re working properly before you begin treatment.
You may also have some scans to check where the cancer has spread to. These may include a bone scan, an MRI (magnetic resonance imaging) scan, a PET (positron emission tomography) scan, or a CT (computerised tomography) scan.
If you’re on hormone therapy, you may have a different type of scan to check whether any areas of bone tissue have become weak from osteoporosis. You may hear this called a DEXA (dual energy X-ray absorptiometry) scan or a bone density scan. Your doctor or nurse will be able to give you more information about these.
You will need to visit a dentist before you start treatment. This is because bisphosphonates can occasionally cause jaw problems. If you need dental treatment, you may not be able to have bisphosphonates until your dental treatment has finished. Speak to your doctor or nurse about any health or dental problems you’ve had in the past. Let them know about any medicines you are taking.
During treatment
Bisphosphonates may be given as tablets (oral bisphosphonates) or through a drip into a vein in the arm (intravenous bisphosphonates).
Remember that each hospital and doctor will do things slightly differently. Your doctor will tell you which type of bisphosphonate is most suitable for you and how often you will have treatment.
The most common bisphosphonate given to men with advanced prostate cancer is called zoledronic acid (Zometa®). It is given through a drip into a vein in the arm.
Make sure you drink plenty of water before each treatment – this can help lower your risk of getting kidney problems. Advice varies, but your doctor or nurse may suggest drinking 500ml of water (about two glasses).
The needle in your arm may feel uncomfortable during the treatment, but it shouldn’t hurt. Each treatment session takes about 15 minutes. You might feel dizzy or get flu-like symptoms for around 24 hours after your treatment. Ask your doctor or nurse about ways to manage this – they may suggest taking a mild pain-relieving drug, such as paracetamol. It may also be a good idea to take a friend or family member with you in case you need help getting home afterwards.
How often you have treatment may depend on whether you’re having bisphosphonates to prevent broken bones or for osteoporosis.
- If you’re having bisphosphonates to prevent broken bones, you may have treatment every three or four weeks. Research has found that having treatment every 12 weeks can work just as well, but this isn’t very common.
- If you’re having bisphosphonates for osteoporosis, you may have your treatment every 6 or 12 months.
If you’re also having chemotherapy to treat your prostate cancer, you might be given your bisphosphonate treatment at your chemotherapy appointments. If you miss a treatment, it’s usually fine to continue at your next appointment. This shouldn’t cause you any problems.
Most men don’t have problems with zoledronic acid, but if you do, you might be offered bisphosphonate tablets instead.
The most common bisphosphonate tablets for men with osteoporosis are alendronic acid (Fosamax®) and risedronate sodium (Actonel®). It’s important to read the instructions carefully and do the following things when taking bisphosphonate tablets.
- Take the tablet at the start of the day, at least 30 minutes before you eat, drink or take any other medicines or supplements.
- Take the tablet with a full glass of water (at least 200ml). This must be plain tap water – mineral water, or water with anything added to it, can interfere with the medicine.
- Swallow the tablet whole – don’t suck, crush or chew it.
- Stand up or sit upright in a chair for 30 minutes after taking the tablet to help make sure the tablet is swallowed properly – don’t lie down.
- Don’t eat for at least 30 minutes after taking the tablet.
Alendronic acid and risedronate sodium are taken once a week. If you forget to take the tablet on the usual day, take it on the first morning after you remember. Do not take more than one tablet a day.
Ask your doctor or nurse if you’re not sure when to take your tablets.
How long will I need bisphosphonates?
This will depend on your own situation, and on whether you’re having bisphosphonates for osteoporosis, bone pain or hypercalcaemia.
If you’re having bisphosphonates to treat bone thinning or bone pain, you’ll usually have them for as long as they’re working. Your doctor will probably review your treatment about every two years, or more regularly at your routine appointments, to check it’s working well and not causing you any problems.
If you’re having bisphosphonates to treat hypercalcaemia, you’ll usually stop treatment once your calcium levels are back to normal.
Some bisphosphonates can cause the levels of minerals in your blood, such as calcium, magnesium and phosphate, to become low. These are minerals that the body uses to make new bone. So you’ll have regular blood tests to check you have enough of these minerals. If your levels are low, you may need to take supplements. Some doctors might offer you calcium and vitamin D supplements as soon as you start having bisphosphonates. Your doctor or nurse can tell you more about this.
What are the side effects of bisphosphonates?
Like all treatments, bisphosphonates can cause side effects. The side effects of bisphosphonates can vary from person to person, but they’re usually mild and will last for as long as you’re having them. Ask your doctor or nurse for more information before you begin your treatment.
We describe some of the possible side effects below. Tell your doctor or nurse if you get any of these. There are usually treatments or ways to manage them. But if your side effects start causing you serious problems or they affect your daily life, your doctor might suggest you stop taking the bisphosphonates.
Common side effects
Flu-like symptoms
You may get a high temperature, headache, chills, and muscle and joint pain with some bisphosphonate treatments. This usually only lasts around 24 hours and should go away after the first or second treatment.
Feeling sick (nausea) and being sick (vomiting)
You may feel or be sick after having bisphosphonates. This shouldn’t last for more than a few days. It is more common with zoledronic acid and risedronate sodium than with alendronic acid.
Loss of appetite
You may feel less hungry after having treatment. This should improve in a few days. It’s important to drink lots of water and eat a healthy balanced diet while you’re having bisphosphonates. This can help to prevent health problems, includin kidney problems. Tell your doctor or nurse if your appetite doesn’t improve. They can suggest ways of dealing with this.
Increased pain
Some men get slightly more joint, muscle or bone pain when using bisphosphonates. This can happen with most bisphosphonates, but is more common with alendronic acid. The pain can begin days or months after starting treatment. Pain-relieving drugs can help, but speak to your doctor or nurse if the pain doesn’t improve after a few days.
Kidney problems
Bisphosphonates can change how well your kidneys work. These changes could be serious, so you’ll have regular blood tests to check this. Your kidneys will return to normal if you stop using bisphosphonates.
Stomach or bowel problems
You may get some stomach pain or changes in your bowel habits. For example, you may have loose and watery bowel movements (diarrhoea). Or you may find it hard to empty your bowels (constipation). This is more common if you’re taking bisphosphonate tablets, rather than a drip.
Less common side effects
Rash or itching
You may get a rash on your skin or feel quite itchy. This can be uncomfortable but shouldn’t last more than a few days. Itching is more common with alendronic acid.
Red or sore eyes
Your eyes may feel itchy, sore or dry. You may also experience some blurred vision or general sensitivity to your eyes. Your doctor or nurse can give you eye drops to help with this. This is more common if you’re having zoledronic acid.
Risk of heart problems and stroke
Bisphosphonates may slightly increase your risk of heart problems (including a fast and irregular heartbeat) and stroke. Talk to your doctor about this if you’re worried, or if you’ve had heart problems before.
Jaw bone problems (osteonecrosis of the jaw)
This is when healthy bone tissue in the jaw becomes damaged and dies. Although jaw bone problems are more likely in people using bisphosphonates, it still isn’t very common, particularly if you’re taking bisphosphonate tablets.
The following things may increase your risk of getting jaw bone problems.
- Gum disease, problems with dentures and some dental treatments. Visit your dentist before starting bisphosphonates and let them know you’ll be having this treatment. You may want to show them this fact sheet. Tell your doctor or nurse about any dental problems you have before starting treatment, such as loose teeth, gum problems (pain, swelling or infections) and numbness or heaviness in the jaw. Make sure you keep your teeth and mouth clean. It’s important to visit the dentist regularly while you’re having bisphosphonates, and to tell your doctor if you get any dental problems while you’re having bisphosphonates.
- Smoking. If you smoke, try to stop or smoke less. For information on stopping smoking, talk to your doctor or nurse or visit the NHS website.
- Some medicines. Ask your doctor or nurse if any of the medicines you are taking can increase your risk of getting jaw problems.
Treatment for osteonecrosis of the jaw includes pain-relieving drugs and antibiotics. It will also help if you stop taking bisphosphonates. You may be referred to a specialist.
If you get any unusual side effects from your treatment, tell your doctor or nurse.
You can also visit the Medicines and Healthcare products Regulatory Agency (MHRA) website to report unusual side effects, or call them on 020 3080 6000.
Keeping your bones healthy
A healthy lifestyle is important for your bone health. Try to eat a healthy balanced diet and do regular physical activity, including gentle resistance exercise. Try using light weights or elastic resistance bands. This may be particularly good if you’re on hormone therapy and at risk of bone thinning or weakness.
But remember if you have weak bones, you’re more likely to break a bone if you fall. It’s important to always speak to your doctor or nurse before starting any new exercise, to make sure it’s safe for you to do.
Drinking a lot of alcohol and smoking can increase your risk of bone thinning, so if you smoke try to stop and follow the government’s guidelines on alcohol.
Questions to ask your doctor or nurse
You may find it helpful to keep a note of any questions you have to take to your next appointment.
- Are bisphosphonates suitable for me?
- How often will I have treatment, and for how long?
- What are the main benefits of bisphosphonates?
- What are the main side effects of bisphosphonates, and who do I contact if I get any?
- Am I likely to get osteonecrosis of the jaw?
- What other treatments are available to strengthen my bones?
- Should I take any supplements while I am on bisphosphonates?
- What types of physical activity are safe for me to do?
- Can you refer me to an occupational therapist if I need one?
Dealing with prostate cancer
Being diagnosed and living with prostate cancer can change how you feel about life. If you or your loved one is dealing with prostate cancer you may feel scared, stressed or even angry. There is no ‘right’ way to feel and everyone reacts differently.
Read more about living with advanced prostate cancer, or speak to our Specialist Nurses. They are here to support you and your family.
You may also find it helpful to visit our wellbeing hub for information to help support you in looking after your emotional, mental, and physical wellbeing. If you are close to someone with prostate cancer, find out more about how you can support someone with prostate cancer and where to get more information.
References and reviewers
Updated: June 2022 | Due for Review: May 2025
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management. 2021.
- British Uro-oncology Group (BUG), British Association of Urological Surgeons (BAUS). Multi-disciplinary Team (MDT) Guidance for Managing Prostate Cancer. 2013.
- Serpa Neto A, Tobias-Machado M, Esteves MAP, Senra MD, Wroclawski ML, Fonseca FLA, et al. Bisphosphonate therapy in patients under androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. Prostate cancer and prostatic diseases. 2012;15(1):36–44.
- Patrick DL, Cleeland CS, von Moos R, Fallowfield L, Wei R, Öhrling K, et al. Pain outcomes in patients with bone metastases from advanced cancer: assessment and management with bone-targeting agents. Supportive Care in Cancer [Internet]. 2014 Dec 23 [cited 2015 Feb 18]; Available from: http://link.springer.com/10.1007/s00520-014-2525-4
- Macherey S, Monsef I, Jahn F, Jordan K, Yuen KK, Heidenreich A, et al. Bisphosphonates for advanced prostate cancer. Cochrane Database of Systematic Reviews [Internet]. 2017 Dec 26 [cited 2018 Jan 5]; Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006250.pub2/abstract
- Felice FD, Piccioli A, Musio D, Tombolini V. The role of radiation therapy in bone metastases management. Oncotarget. 2017 Jan 26;8(15):25691–9.
- Mundy GR, Roodman GD, Smith MR. New Opportunities for the Management of Cancer-Related Bone Complications. 2009 [cited 2013 Nov 4]; Available from: http://www.curatio-cme.com/newsletters/CAHO_New_Opp_May2009.pdf
- Gastanaga VM, Schwartzberg LS, Jain RK, Pirolli M, Quach D, Quigley JM, et al. Prevalence of hypercalcemia among cancer patients in the United States. Cancer Medicine. 2016 Aug;5(8):2091–100.
- Scottish Medicines Consortium. Zoledronic acid (Zometa®) [Internet]. 2004 [cited 2015 May 13]. Available from: https://www.scottishmedicines.org.uk/SMC_Advice/Advice/Zoledronic_acid__Zometa__-_Independent_Review/Zoledronic_acid__Zometa___IPR
- Attar S, Steffner RJ, Avedian R, Hussain WM. Surgical intervention of nonvertebral osseous metastasis. Cancer Control. 2012;19(2):113–21.
- National Institute for Health and Care Excellence. Percutaneous cementoplasty for palliative treatment of bony malignancies. IPG179. 2006;
- Healthcare Improvement Scotland. Denosumab for the prevention of skeletal-related events in adults with bone metastases from solid tumours. NICE (Multiple) Technology Appraisal Guidance No 265 [Internet]. [cited 2015 May 13]. Available from: http://www.healthcareimprovementscotland.org/programmes/nice_guidance_and_scotland/mta_resources/appraisal_265.aspx?iru=FV15K62K54
- Wenter V, Herlemann A, Fendler WP, Ilhan H, Tirichter N, Bartenstein P, et al. Radium-223 for primary bone metastases in patients with hormone-sensitive prostate cancer after radical prostatectomy. Oncotarget. 2017 Apr 21;8(27):44131–40.
- Todenhöfer T, Stenzl A, Hofbauer LC, Rachner TD. Targeting Bone Metabolism in Patients with Advanced Prostate Cancer: Current Options and Controversies. International Journal of Endocrinology. 2015;2015:1–9.
- Sottnik JL, Keller ET. Understanding and targeting osteoclastic activity in prostate cancer bone metastases. Current molecular medicine. 2013;13(4):626–39.
- Abrahamsen B, Brask-Lindemann D, Rubin KH, Schwarz P. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. BoneKEy Reports. 2014 Sep 3;3:574.
- Singh T, Kaur V, Kumar M, Kaur P, Murthy RSR, Rawal RK. The critical role of bisphosphonates to target bone cancer metastasis: an overview. Journal of Drug Targeting. 2015 Jan 2;23(1):1–15.
- Porta-Sales J, Garzón-Rodríguez C, Llorens-Torromé S, Brunelli C, Pigni A, Caraceni A. Evidence on the analgesic role of bisphosphonates and denosumab in the treatment of pain due to bone metastases: a systematic review within the European Association for Palliative Care guidelines project. Palliative medicine. 2017;31(1):5–25.
- Zoledronic acid 4 mg/5 ml concentrate for solution for infusion - Summary of Product Characteristics (SmPC) - (emc) [Internet]. [cited 2022 Feb 7]. Available from: https://www.medicines.org.uk/emc/product/11461/smpc#gref
- electronic Medicines Compendium. Zometa 4mg/5ml Concentrate for Solution for Infusion [Internet]. [cited 2015 Feb 24]. Available from: http://www.medicines.org.uk/EMC/medicine/14062/SPC/Zometa+4mg+5ml+Concentrate+for+Solution+for+Infusion/
- Overview | Osteoporosis: assessing the risk of fragility fracture | Guidance | NICE [Internet]. NICE; [cited 2022 Feb 7]. Available from: https://www.nice.org.uk/guidance/cg146
- National Institute for Health and Clinical Excellence. Osteoporosis: assessing the risk of fragility fracture. Short clinical guideline. Clinical guideline 146 [Internet]. 2012 [cited 2015 Nov 16]. Available from: https://www.nice.org.uk/guidance/cg146/evidence/osteoporosis-fragility-fracture-full-guideline-186818365
- Spanou A, Lyritis G, Chronopoulos E, Tournis S. Management of bisphosphonate-related osteonecrosis of the jaw: a literature review. Oral Diseases. 2015 Nov;21(8):927–36.
- Reyes C, Hitz M, Prieto-Alhambra D, Abrahamsen B. Risks and Benefits of Bisphosphonate Therapies. Journal of Cellular Biochemistry. 2016 Jan;117(1):20–8.
- Beth-Tasdogan NH, Mayer B, Hussein H, Zolk O. Interventions for managing medication-related osteonecrosis of the jaw. Cochrane Oral Health Group, editor. Cochrane Database of Systematic Reviews [Internet]. 2017 Oct 6 [cited 2022 Feb 7];2017(10). Available from: http://doi.wiley.com/10.1002/14651858.CD012432.pub2
- Himelstein AL, Foster JC, Khatcheressian JL, Roberts JD, Seisler DK, Novotny PJ, et al. Effect of Longer-Interval vs Standard Dosing of Zoledronic Acid on Skeletal Events in Patients With Bone Metastases: A Randomized Clinical Trial. JAMA. 2017 Jan 3;317(1):48.
- National Institute for Health and Care Excellence. Bisphosphonates for treating osteoporosis. Technology appraisal guidance 464. 2017.
- Medicines and Healthcare products Regulatory Agency (MHRA). Bisphosphonates: use and safety [Internet]. 2014 [cited 2018 Jan 8]. Available from: https://www.gov.uk/government/publications/bisphosphonates-use-and-safety/bisphosphonates-use-and-safety
- Fosamax Once Weekly 70mg Tablets - Summary of Product Characteristics (SmPC) - (emc) [Internet]. [cited 2022 Feb 7]. Available from: https://www.medicines.org.uk/emc/product/1281/smpc
- Risedronate Sodium Accord Once a Week 35mg film-coated tablets - Patient Information Leaflet (PIL) - (emc) [Internet]. [cited 2022 Feb 7]. Available from: https://www.medicines.org.uk/emc/product/6757/pil
- Body JJ, von Moos R, Niepel D, Tombal B. Hypocalcaemia in patients with prostate cancer treated with a bisphosphonate or denosumab: prevention supports treatment completion. BMC Urology. 2018 Sep 20;18(1):81–81.
- Electronic Medicines Compendium. Fosamax - Summary of Product Characteristics [Internet]. [cited 2017 Jul 12]. Available from: https://www.medicines.org.uk/emc/medicine/1175#UNDESIRABLE_EFFECTS
- Electonic Medicines Compendium. Actonel 30 mg film-coated tablets - Summary of Product Characteristics [Internet]. 2016 [cited 2017 Jul 12]. Available from: https://www.medicines.org.uk/emc/medicine/3341#UNDESIRABLE_EFFECTS
- Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O’Ryan F, et al. Diagnosis and Management of Osteonecrosis of the Jaw: A Systematic Review and International Consensus. Journal of Bone and Mineral Research. 2015 Jan;30(1):3–23.
- Lee SH, Chan RC, Chang SS, Tan YL, Chang KH, Lee MC, et al. Use of bisphosphonates and the risk of osteonecrosis among cancer patients: a systemic review and meta-analysis of the observational studies. Supportive Care in Cancer. 2014 Feb;22(2):553–60.
- Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, et al. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;8:CD007566.
- Owen PJ, Daly RM, Livingston PM, Fraser SF. Lifestyle guidelines for managing adverse effects on bone health and body composition in men treated with androgen deprivation therapy for prostate cancer: an update. Prostate Cancer Prostatic Dis. 2017 Jun;20(2):137–45.
- Cormie P, Galvão DA, Spry N, Joseph D, Chee R, Taaffe DR, et al. Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: a randomised controlled trial. BJU Int. 2015;115(2):256–66.
- Grossmann M, Hamilton EJ, Gilfillan C, Bolton D, Joon DL, Zajac JD. Bone and metabolic health in patients with non-metastatic prostate cancer who are receiving androgen deprivation therapy. Med J Aust. 2011;194(6):301–6.
- Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, et al. Effects of resistance exercise in prostate cancer patients: a meta-analysis. Supportive Care in Cancer. 2017 Jun 10;
- Thorsen L, Courneya KS, Stevinson C, Fosså SD. A systematic review of physical activity in prostate cancer survivors: outcomes, prevalence, and determinants. Supportive Care in Cancer. 2008 Feb 15;16(9):987–97.
- Baumann FT, Zopf EM, Bloch W. Clinical exercise interventions in prostate cancer patients: a systematic review of randomized controlled trials. Supportive Care in Cancer. 2012;20(2):221–33.
- Keogh JWL, MacLeod RD. Body Composition, Physical Fitness, Functional Performance, Quality of Life, and Fatigue Benefits of Exercise for Prostate Cancer Patients: A Systematic Review. Journal of Pain and Symptom Management. 2012 Jan;43(1):96–110.
- Department of Health. UK Chief Medical Officers’ Low Risk Drinking Guidelines. 2016.
- Vanessa Basketter, Urology Nurse Specialist, University Hospital Southampton
- Maggie Bingle, Prostate Cancer Clinical Nurse Specialist, East Suffolk and North Essex NHS Foundation Trust
- Our Specialist Nurses
- Our volunteers.


