Making the case for Clinical Nurse Specialists
The Clinical Nurse Specialist (CNS) workforce is declining, the number of men diagnosed with prostate cancer is rising and the provision of CNSs across the UK is uneven. The need to grow the number of prostate cancer specialist nurses is greater than ever.
We want every man with prostate cancer to have access to a named CNS, who can provide the specific support he needs. NICE recommendations and results from the National Cancer Patient Experience Survey (NCPES) support this model of care.
We've produced a guide for decision makers to help you develop a strategic plan for CNSs in prostate cancer care. We've surveyed CNSs across the UK to better understand the CNS workforce in 2019. We've looked at existing access to a CNS, improving access and the benefits of patients having a named CNS.
The evidence
Existing access
Men’s access to a clinical nurse specialists varies across the UK (13). For the CNS workforce to support all men, we need to understand how variation in CNS access exists across the UK (14). In some parts of England only 60 per cent of men with prostate cancer are given access to a named CNS (13). We want to see the recommendations outlined in the 2015 cancer strategy Achieving World-Class Cancer Outcomes implemented to ensure “access to a CNS or other key worker for all patients”(17).
CNS numbers in the UK:
- England - 463 in 2018, 510 needed by 2028*
- Scotland - 26.5 in 2018, 59 needed by 2028*
- Wales - 26 in 2018, 32 needed by 2028*
- Northern Ireland - 4 in 2018, 26 needed by 2028*
* This number is based on Prostate Cancer UK’s population projections of the number of men who will be living with prostate cancer in 2028 in the UK and the CNSs needed to support them. Figures are estimated using the caseload assumptions described in the Department of Health commissioned Frontier Economic Report (16).
The number of urology CNSs is lower than other cancer types. In 2017, the Macmillan Census reported that 12 per cent of CNSs in England are specialised in urology, compared with 18 per cent in breast cancer. Based on cancer prevalence, that suggests that each breast cancer CNS in England has a caseload of approximately 160 patients, whereas for urological cancers, the caseload is around 795 cases per urology CNS (3,11). We want to see more CNSs specialised in prostate cancer care to give men the care they deserve.
The future will present further challenges for us, with increasing volume of patients, which will increase the pressure on all services.
Improving access
To ensure more men have access to a CNS, we need to increase the number of CNSs across the UK so that wherever a man lives, he will have access to a CNS during his prostate cancer treatment journey. How a CNS delivers health care is changing and more is now required from a CNS, making it particularly important for decision makers to focus on CNS recruitment, development and retention.

Why improve access?
As well as being a key worker and a source of expert knowledge, a CNS has a focus on providing vital emotional support. CNSs take a holistic approach to care incorporating physical, social, and psychological wellbeing; not just the condition alone.
UK-wide cancer patient experience surveys have demonstrated that having access to a CNS has a statistically significant impact on patient experience and understanding of the disease (8-10). The 2017 English National Cancer Patient Experience Survey report found that 71 per cent of patients with prostate cancer said that all or most of the time their CNS answered their important questions in a way they could understand. The results from the survey showed that patients with a CNS are less likely to feel isolated and more likely to feel that they have their information needs met and are in control of their own decisions.
Patients with access a CNS reported feeling: (14),(20)
- Informed about routine tests, their results and other support services;
- Supported at diagnosis with a point of contact to answer questions;
- Having access to information;
- Consulted about treatment options and able to make informed decisions;
- Confident in their GP and nurse;
- Treated with dignity and respect.
Taking a holistic approach
CNSs are essential to develop and deliver innovative and cost-effective forms of support for prostate cancer patients. Internet-based follow up and Telehealth can provide access for harder to reach men. Patient-supported self-management is not only cost-effective in comparison to hospital-based follow up, but can help men feel in control of their own care. TrueNTH have developed resources to support health services to implement CNS supported patient self-management.
Survivorship programmes can also help to reach men by supporting their individual needs after they have undergone radical treatments. We want to support CNSs in delivering survivorship programmes and have developed an e-learning module.
Patients can be further supported with a Holistic Needs Assessment (HNA) (21), although this is not always possible - often due to workload. The HNA enables a CNS to determine a level of distress, despite how calm the patient may seem. It helps to identify the patient’s initial concerns, and it can be instrumental in providing the best support and care for men.
Men with prostate cancer discuss treatment options and adverse effects with a named nurse specialist.
Case study: Simon
Simon is one of the 47,000 men diagnosed with prostate cancer each year. Simon works as a personal trainer alongside a CNS to support men recovering from prostate cancer and champions the need for all men with prostate cancer to have access to a CNS.
Simon was diagnosed with prostate cancer at the age of 50 and throughout his treatment journey was fully supported by the same CNS. Simon found the support he received invaluable and it helped him feel more confident and reassured at what can be a stressful time for many men.
Growing the CNS workforce
We know that 49 per cent of nurses surveyed working within urology have said that they are eligible for retirement or are intending to leave the profession within the next 10 years (25). The need for decision makers to grow the CNS workforce is greater than ever. Decision makers need to focus on a proactive approach to recruitment, development and retention of prostate cancer specialist nurses.
The Health Service Journal (HSJ) published an editorial on the benefits of the specialist nurse workforce. Nurses help in efficiency, leadership, service redesign, service improvement, development of the workforce and improving patient experience. These benefits out-weigh the cost of the specialist nurse (22).
We’ve put together a template job description as a recruitment tool, listing all the key skills a CNS should bring.
Mature succession planning and recruiting to replace any CNSs leaving the service needs to be implemented by decision makers to ensure the CNS workforce is sustainable. As well as replacing CNSs leaving the profession, recruiting staff for administrative support for all specialist nurses would be cost-saving and allow CNSs more time for clinical duties.
Offer men with prostate cancer individualised information tailored to their own needs. This should be given by a healthcare professional (for example, a specialist nurse)
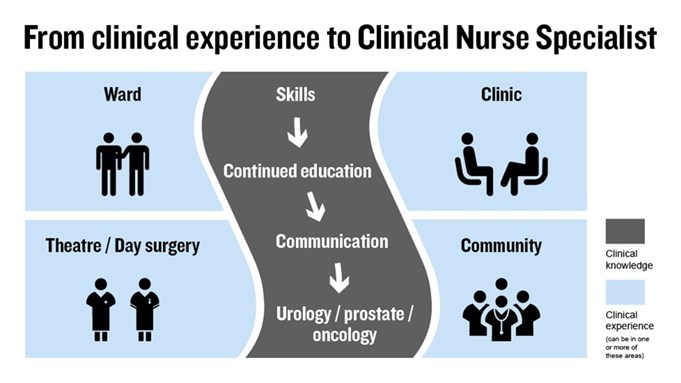
Developing CNSs
CNSs carry out a wide-range of tasks, making them a key member of the multi-disciplinary team (MDT). They provide expert advice on a range of issues including symptom control. They deliver treatment, provide continuity of care, develop post-treatment plans and are a key contact for patients. CNSs provide clincally complex care which includes, performing digital rectal examinations (DREs) and biopsies, advice on treatment options and assist during surgical procedures.
A CNS can also learn on the job:
- Lower urinary tract symptoms (LUTS) assessment;
- Catheterisation;
- Interpreting and understanding prostate specific antigen (PSA) levels
- Understanding of clinical trials that influence prostate cancer and current recruiting trials
- Survivorship issues - follow up, appropriate specialist support services (erectile dysfunction, continence) and signs of recurrence.
Provision of CNSs across the UK varies: there are many unfilled CNS posts and not currently enough nurses with the expertise to fill them, often making the creation of new CNS roles necessary (14). Investing in training and education is essential to enable nurses to reach the level of skills and knowledge required to fulfill the CNS role. We provide tailored education events to support CNSs and offer bursaries to encourage nurses to specialise in prostate cancer care.
Retaining CNSs
Nurse-led care produces the same level care at lower cost (23). Professor Alison Leary, Healthcare and Workforce Modelling Lead at London South Bank University, studied 12,000 specialist nurses in advanced practice, for around 50 million hours of work. This found specialist nurses to be a cost effective, high quality option in delivering care by demonstrating high levels of expertise, proactive case management, identifying problems before they arise and avoiding unnecessary admissions (22). We want to see more organisations using the knowledge CNSs have and utilising their potential as nurses to successfully lead services.
To continue to provide good service to men, trusts need to focus on retention. Decision makers need to develop mature succession planning, to account for any changes in staff before the service is left underresourced.
To grow our workforce, more education opportunities and support in career progression is needed so we have capacity to treat men with prostate cancer in the future.
Next steps
The benefits of a CNS are clear. A CNS workforce provides a safe, consistent, cost-effective and high quality service. However, the future of the CNS workforce is not stable, with 49 per cent of nurses within urology due to leave or retire, within the 10 next years. We are calling on decision makers to plan for the future of CNSs.
We’re here to support decision makers to take action. The Prostate Cancer UK Best Practice Pathway is a resource to allow you make decisions on how to commission and properly resource services as well as support and deliver the best treatment and care to men. We also offer education support to develop CNSs through bursaries and an education programme of face to face and online learning to encourage career progression.
Our recommendations for embedding CNSs in a multidisciplinary team (MDT):
- Plan a strategic workforce design through effective investment, training and education;
- Develop mature succession planning;
- Provide administrative support for all specialist nurses so they have more time for clinical duties;
- Invest in training to support the leadership skills of your CNS workforce to enable nurse-led services.
- ISD Scotland. Cancer Statistics: Male Genital Organ Cancer Incidence, Mortality, Prevalence, Survival . 2018. [Cited 2018]. Available from: http://www.isdscotland.org/Health-Topics/Cancer/Cancer-Statistics/Male-Genital-Organs/
- Queen’s University Belfast N. Ireland Cancer Registry.. N. Ireland Cancer Registry Incidence, Mortality, Survival 2016.2018. . [Cited 2018]. Available from: https://www.qub.ac.uk/research-centres/nicr/CancerInformation/official-statistics/BySite/Prostatecancer/
- Public Health England and Macmillan. Cancer Prevalence in England: 21 year prevalence by demographic and geographic measures. 2018. [Cited 2018]. Available from: http://www.ncin.org.uk/about_ncin/segmentation
- Macmillan and WCISU partnership. Cancer incidence and prevalence for cluster networks in Wales. 2018. [Cited 2018] Available from Tableau.
- Cancer Research UK. Cancer incidence for common cancers. 2018 [cited 2019]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence/common-cancers-compared#heading-One
- Mistry M, Parkin DM, Ahmad AS and Sasieni P. Cancer incidence in the United Kingdom: projections to the year 2030. Br J Cancer. 2011 Nov 22;105(11):1795–803.
- Health Services Journal. Workforce supplement: The benefits of specialist nurses. 2015. [cited 2019]. Available from: https://www.hsj.co.uk/supplement-archive/workforce-supplement-the-benefits-of-specialist-nurses/5082712.article?blocktitle=Supplement&contentID=15038#.VPXnasZ4h3M
- Quality Health and NHS England. National Cancer Patient Experience Survey 2013: National report. 2013. [Cited 2019] Available from: https://www.quality-health.co.uk/resources/surveys/national-cancer-experience-survey/2013-national-cancer-patient-exerience-survey/2013-national-cancer-patient-experience-survey-reports/301-2013-national-cancer-patient-experience-survey-programme-national-report/file
- Public Health Agency, Macmillan and Quality Health. Northern Ireland Cancer Patient Experience Survey. 2015. [cited 2019]. Available from: https://www.quality-health.co.uk/resources
- Macmillian and Picker. National Report: Wales Cancer Patient Experience Survey 2016. 2017. [cited 2019]. Available from: https://gov.wales/docs/dhss/publications/170705national-reporten.pdf
- Cancer Workforce in England. 2017.[Cited 2019]. Available from: https://www.macmillan.org.uk/_images/cancer-workforce-in-england-census-of-cancer-palliative-and-chemotheraphy-speciality-nurses-and-support-workers-2017_tcm9-325727.pdf
- National Institute for Health and Care Excellence, Prostate cancer: diagnosis and management [CG175] Measuring the use of this guidance. 2016. [Cited 2019]. Available from: https://www.nice.org.uk/guidance/CG175/uptake
- Quality Health and NHS England. National Cancer Experience Patient Survey 2017: Trust level results. 2017 [cited 2019]. Available from: http://www.ncpes.co.uk/reports/2017-reports/local-reports-2/trusts-2
- Macmillian and NHS. Quality in Nursing Excellence in Cancer Care: The contribution of the Clinical Nurse Specialist. 2010. [cited 2019]. Available from: https://www.macmillan.org.uk/documents/aboutus/commissioners/excellenceincancercarethecontributionoftheclinicalnursespecialist.pdf
- Frontier Economics, One to one support for cancer patients: A report prepared for the Department of Health. 2010. [Cited 2019]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216683/dh_122521.pdf
- Griffiths P, Simon M, Richardson A and Corner, J. Is a large specialist nurse workforce in cancer associated with better patient experience? Cross-sectional study. J Health Serv Res Policy. 2013; 18 (Suppl 1): 39-46.
- National Health Service. Achieving World-Class Cancer Outcomes: A Strategy for England 2015-2020 – Progress Resport 2016-2017. 2017. [Cited 2019]. Available from: https://www.england.nhs.uk/wp-content/uploads/2017/10/national-cancer-transformation-programme-2016-17-progress.pdf
- Cancer Research UK, Cancer mortality for common cancers. 2016. [cited 2019]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/mortality/common-cancers-compared#heading-Zero
- Henry R. The Role of the Cancer Nurse Specialist. Nursing in Practice. 2015; [cited 2019]. Available from:https://www.nursinginpractice.com/article/role-cancer-specialist-nurse
- Doyle N and Henry R. Holistic Needs Assessment: Rationale and Practical Implementation. Cancer Nursing Practice. 2014. 13(5): 16-21
- Health Services Journal Workforce, Time For Some Advanced Thinking? The benefits of Specalist Nurses. Feb 2015; 27. [cited 2019]. Available from: https://www.hsj.co.uk/download?ac=1298457
- Ndosi M, Lewis M, Hale C, Quinn H, Ryan S, Emery P, Bird H and Hill J. The outcome and cost-effectiveness of nurse-led care in people with rheumatoid arthritis: a multicentre randomised control trial. Ann Rheum. 2013; 73:1975-1982.
- Leary A, Brocksom J, Endacott R, et al. The Specialist nursing workforce caring for men with prostate cancer in the UK. International Journal of Urological Nursing. 2016. 10(1): 5-13

