Best Practice Pathway
We want every man with prostate cancer – or at risk of it - to have access to the same high-quality diagnosis, treatment and care, no matter where in the UK he lives.
The Prostate Cancer UK Best Practice Pathway makes this possible.
Please be aware the Best Practice Pathway is currently under review and will be updated shortly to reflect recent changes in diagnosis, treatment and support. If, in the meantime, you have any questions regarding the pathway please get in touch with our policy team.
The big idea
Developed to support healthcare professionals at the front line of prostate cancer diagnosis and care, our Best Practice Pathway uses easy to follow flowcharts to guide healthcare professionals deliver best practice diagnosis, treatment and support. It sets out how to achieve an early diagnosis in men at higher than average risk of the disease. It also supports use of the most up-to-date, cutting-edge research-led innovations - so that healthcare professionals are equipped and supported to provide the very latest evidence-based best practice to their patients.
1) The diagnostic pathway
The Diagnostic Pathway has been developed by leading Urology teams at UCLH, the Christie and Royal Marsden Cancer Vanguards brought together by NHS England and supported by Prostate Cancer UK. It uses evidence from the PROMIS trial and recent innovative one-stop shop prostate cancer diagnostic pilots to create a prostate cancer diagnostic pathway that can deliver to the new time to diagnosis standard of 28 days.
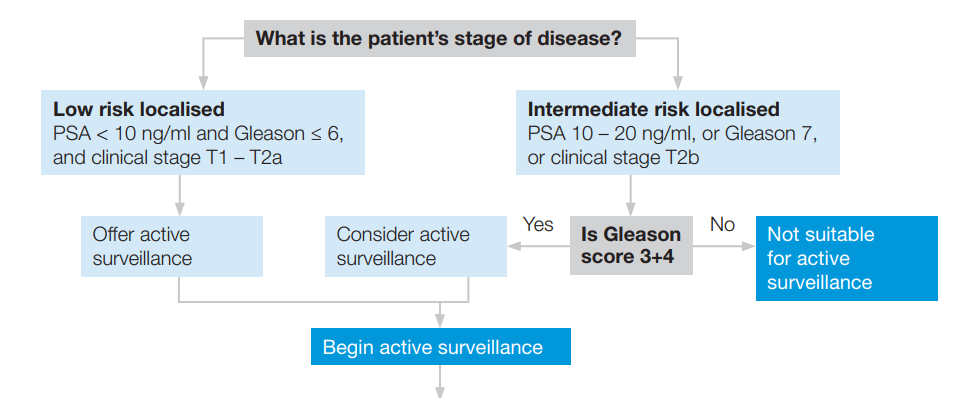
Extract from Best Practice Pathway: Treatment, Active Surveillance
2) The treatment pathway
Just as every man is an individual, every treatment pathway is individual and needs to be tailored to the needs of the man. Each man must have the opportunity to make an informed choice about their treatment pathway, having been given detailed information about the treatments available for the stage of their disease, the side effects associated with each of these treatments and the outcomes the treatments will provide. For men with low risk cancer, active surveillance must be presented as a treatment option alongside surgery and radiotherapy.
3) The support pathway
A prostate cancer diagnosis and its treatments can cause men psychological and physical side-effects that require supportive care. The Support Pathway outlines the breadth of potential side-effects that men can experience while providing detailed guidance on the best practice care and support that can enable these men to achieve a better quality of life. It also offers innovative solutions for stratified follow-up and sets out patient behaviour change initiatives that may prevent recurrence or complications resulting from the unmanaged consequences of treatments.
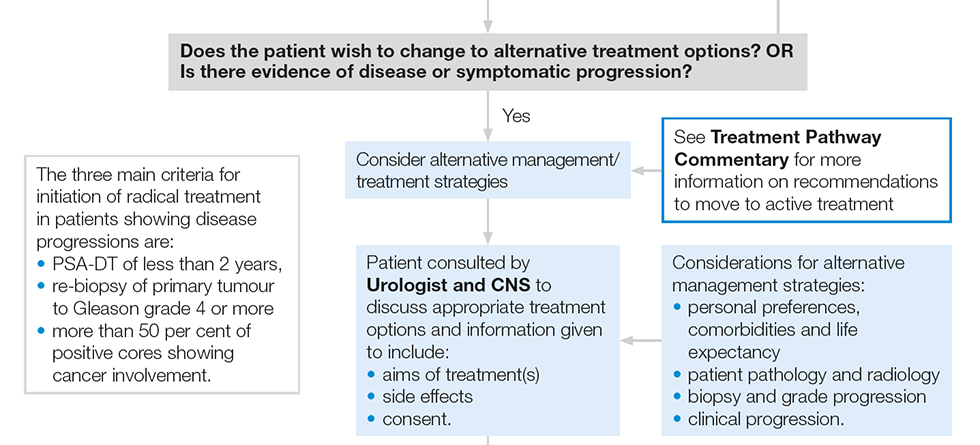
Extract from Best Practice Pathway: Treatment, Active Surveillance
How have we developed it?
Prostate Cancer UK worked with clinical experts from urology, medical and clinical oncology, and radiology. We also secured expert input from clinical nurse specialists, general practitioners and the National Institute for Clinical Excellence (NICE) to develop the Best Practice Pathway.
Thanks to this collaboration, the Support Pathway is endorsed by NICE and aligned with their guidance.
In addition, the Best Practice Pathway has been peer reviewed by a Clinical Reference Group (CRG) that has included representatives from all the relevant professional bodies and leading prostate cancer clinical researchers.
The CRG will continue to work with us to make sure that the best practice pathway remains up-to-date and robust.
Q&A
- We have included new, recently published research that is delivering breakthrough changes in prostate cancer diagnosis and treatment, for example the latest results of the STAMPEDE trial.
- We have aligned with NICE Prostate Cancer Guidelines CG175 recommendations, where they are not superseded by recently published research them.
- We have drawn from our comprehensive Prostate Cancer UK health information resources, which are regularly peer reviewed and certified by the Information Standard, which is a quality mark for reliable health and social care information. This means that we follow best practice when producing health information to make sure that it is up-to-date, evidence-based, clinically accurate, reviewed by people affected by prostate cancer, accessible and easy to read.
- Our medical research programme and the connections we have with the prostate cancer medical research world means our Best Practice Pathway can keep pace with new developments in prostate cancer diagnosis and treatment
- We have first-hand insight into patient experience provided by the thousands of men (and their families) who regularly engage with us and can use this to shape the Best Practice Pathway.
- We want to make sure that the Best Practice Pathway includes new practice changing medical research and other new evidence. That’s why we will aim to update the Best Practice Pathway every 6 months.
