Research
11 Sept 2024More men with advanced prostate cancer could benefit from precision medicine olaparib
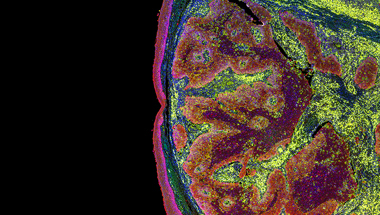
Researchers have found a further group of prostate cancers that could be treated with olaparib - a drug that's transformed treatment for some men with advanced cancer.

Olaparib, a drug that can kill cancer cells with faulty DNA repair mechanisms, could benefit more men than previously thought.
Currently, only men whose cancer has a mutation in its BRCA1 or BRCA2 gene can get olaparib on the NHS.
However, researchers at The Institute of Cancer Research (ICR), supported by Prostate Cancer UK, have found another genetic change in some prostate cancers that could make them susceptible to the treatment.
In a small sample of men whose cancer had this genetic mutation, taking olaparib led to a fall in the number of cancer cells detectable in blood tests - implying the treatment was effective.
Also, the researchers found the genetic change was common in prostate cancer biopsies, suggesting olaparib could benefit many more men than can currently access the treatment.
Targeting cells with faulty repair systems
Originally developed and approved to treat women with breast or ovarian cancer, olaparib can kill cancer cells that have a mutation in one of two genes known as BRCA1 and BRCA2.
These genes help cells repair their DNA – meaning cancer cells that have a faulty version of these genes are more dependent on other ways of repairing their DNA to survive. Olaparib is one of a group of drugs (called PARP inhibitors) that block one of these remaining routes, making the cancer cells more likely to die.
Thanks to your support, we were able to fund research that later found the treatment to be effective in prostate cancer, for men whose cancer also has these faulty repair mechanisms.
However, research since then has suggested that up to 30 per cent of men with advanced prostate cancer have tumours that have faulty DNA repair mechanisms, suggesting more men might benefit from olaparib than we originally thought.

Fall in the number of cancer cells after treatment
The new change found by the team at the ICR is to a gene called RNASEH2B, which also helps cells repair damaged DNA.
After giving olaparib to men with advanced cancer, researchers found the number of cancer cells with this mutation fell in 13 out of 18 men – despite none of them having the usual mutations to their BRCA1 or BRCA2 genes.
This suggests that these cells were successfully being killed off by the treatment.
The team also found that six of these men had fewer cancer cells circulating in their bloodstream after taking olaparib – a further indication that the treatment was working.
In a sign of the potential population of men who could benefit from olaparib, out of 124 men with advanced prostate cancer, the team found 44 per cent were missing a complete copy of the gene in at least half their cancer cells – and 20 per cent had lost the gene in three quarters of their cancer cells.
We already knew that these drugs helped men with mutations in specific genes like BRCA, and this exciting research shows they could also benefit a completely different group of men.
Each man is unique – and so is his prostate cancer
Professor Johann de Bono, Regius Professor of Cancer Research at the ICR, led the research. He said: “We have identified a genomic aberration that is found in some prostate cancers that makes them very vulnerable to a targeted cancer drug, called a PARP inhibitor, which comes in pill form and has much fewer side effects than chemotherapy.
“Further research is urgently needed to validate these findings and the tests that would identify tumours sensitive to PARP inhibitors beyond BRCA gene mutations so we can provide a new treatment option for patients with advanced prostate cancer.”
Our Senior Research Impact and Intelligence Manager, Dr Hayley Luxton, said: “Each man is unique – and so is his prostate cancer – which is why targeted treatments like PARP inhibitors are so important.
“These drugs have already begun to revolutionise the way we treat cancer, moving us away from the old ‘one-size fits all’ approach. And what’s important now is to figure out exactly who will benefit the most.
“We already knew that these drugs helped men with mutations in specific genes like BRCA, and this exciting research shows they could also benefit a completely different group of men whose cancer cells have lost a novel marker called RNASEH2B.
“We’re proud of the role we played in funding this research, which is a result of a bespoke funding scheme we designed to deliver breakthroughs exactly like this one. We now look forward to future research that will identify how we can test for this and make these life-extending drugs available to even more men.”
'I'll be helping to fund research that will one day stop prostate cancer'
Around 1 in 4 of our research projects - just like this one - are funded by gifts in Wills.
David chose to leave us a gift in his Will after his own prostate cancer diagnosis and treatment. He wanted to do something to help other men on the same path.
“A gift in my Will means I can continue to stand for the thing I care most about, even when I’m gone," he said. “Hopefully, I’ll be helping to fund the research that will one day stop prostate cancer altogether.”
We've partnered with the National Free Wills Network, so you can have your Will written or updated for free. You don't have to include a gift to Prostate Cancer UK, but even a small contribution could have a lifechanging impact for generations to come. And we would be forever grateful for your support.