Campaigns
23 Jul 2024The new Government can save lives and smash inequalities – here's how you can make it happen
Outdated NHS guidance on prostate cancer is putting men's lives at risk and making health inequalities worse. That's why we're urging the Government to make prostate cancer a priority.

It’s rare that one simple change could save thousands of lives. But by changing the way GPs talk about prostate cancer, we could do exactly that.
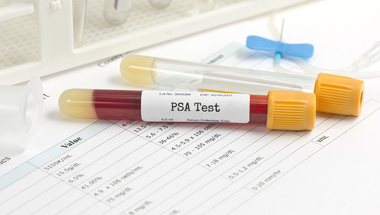
Right now, unless men have symptoms of prostate cancer, they have to ask their GP for a PSA blood test. That’s because GPs are told not to raise the issue with men unless they have symptoms.
But early-stage prostate cancer doesn’t usually cause symptoms, meaning too many men are being diagnosed too late for a cure. More than 10,000 in the UK every year.
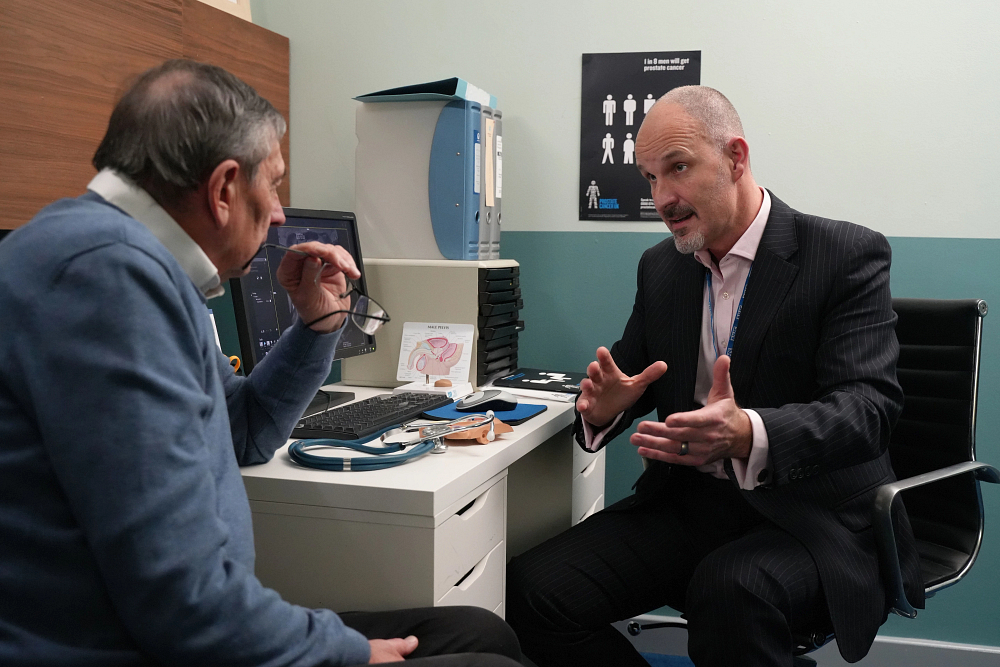
That’s why we’re calling on the new Government to change these outdated NHS guidelines. If primary healthcare professionals (such as GPs and practice nurses) can proactively discuss prostate cancer risk and PSA testing with the men who are most at risk, it could save thousands of men from a late diagnosis.
Our call is backed up by the UK's leading prostate cancer clinicians and experts, who have published a landmark paper in the British Journal of General Practice. They urge the Government to push through changes that would see healthcare professionals starting these potentially life-saving conversations with men at highest risk.
And, most importantly, you’re also calling for change. During the election campaign, nearly 3,000 of you contacted your local candidates, asking them to push for the NHS guidelines to be reformed if elected to parliament. 572 of these candidates are now MPs.
Now we want to see them act – by updating NHS guidance so GPs speak to those at highest risk and men can make an informed choice about the PSA blood test.
The current situation is failing men
Prostate cancer often has no symptoms in its earlier, more treatable stages, so it’s crucial that men know about their risk of getting the disease and think about the option of getting a PSA blood test, even if they feel healthy.
However, in the current system the men who are the most likely to get prostate cancer – including Black men and men with a family history of the disease – aren’t told about their higher risk by GPs.
This situation is particularly failing Black men and men living in poverty. Black men have double the risk of both getting prostate cancer and dying from it, while men living in deprived areas of the UK are 29% more likely to be diagnosed with incurable disease.
Yet we estimate that updating the NHS guidance, and implementing plans for raising awareness about the changes, could be delivered in just 12 months.
Chiara De Biase, our Director of Health Services, Equity & Improvement, said: “This outdated guidance is failing both men and their clinicians – and it’s about time that changed. We want the Government to fix this failing system and start allowing clinicians to have these potentially life-saving conversations with men at highest risk.”
If I’d known to speak to my GP about it earlier and had that conversation, it might have saved me. I hope this leads to a change in guidance so all men can have those sorts of lifesaving conversations.
"I could have had the cancer for 10 years already without having any symptoms"

Tony Collier was diagnosed with stage four prostate cancer in 2017 and told he had just two years to live. He was part of the panel of men with lived experience of prostate cancer who shared their stories to support the drafting of the PSA Consensus paper.
He said: “I was diagnosed with advanced prostate cancer in 2017 after speaking to a sports injuries doctor about what I thought was just a runner's groin strain.
“Unfortunately, it turned out to be far more serious, and the pain was caused by cancer which had spread extensively to my bones. I was originally given just two years to live and was told at the time that I could have had the cancer for 10 years already without having any symptoms.
“I’ve been lucky that new treatments mean I’ve been able to keep the cancer at bay and have now far outlived my original prognosis. That’s why I’m so determined to give back and have worked hard over the years to raise awareness and hopefully save lives by getting more men diagnosed earlier.
“I’m so proud to have been part of such an important project. If I’d known to speak to my GP about it earlier and had that conversation, it might have saved me, and I hope this leads to a change in guidance so all men can have those sorts of lifesaving conversations.”
Leaving men in the dark about their risk means too many men are getting diagnosed with incurable prostate cancer, and this disproportionately affects Black men and men living in deprived areas.
Updating guidance could give men a fairer chance
Historically, the PSA blood test was the subject of disagreement because there are pros and cons to its use as a diagnostic tool – for example, a raised PSA result can be caused by things other than prostate cancer – which used to lead to unnecessary and possibly harmful biopsies.
But today, with the introduction of MRI scans, the way we diagnose prostate cancer is now safer and more accurate than it’s ever been.
Amy Rylance, our Assistant Director of Health Improvement, said: “It’s been clear for some time that NHS guidelines that prevent GPs from raising the subject of prostate cancer are dangerously outdated, and deeply unfair to the men who face double the risk of getting the disease.
“Leaving men in the dark about their risk means too many men are getting diagnosed with incurable prostate cancer, and this disproportionately affects Black men and men living in deprived areas.
“We welcome the new Government’s promises to increase earlier cancer diagnoses and to address gross health inequalities. Our message to the Government and MPs is that we’re here to help you deliver those promises. Updating NHS prostate cancer guidelines could drive forward significant progress in just a year and, crucially, would give men a fairer chance of living longer.”