Research
27 Aug 2021Can we train the immune system to attack prostate cancer? We're funding these researchers to find out.
We’ve invested £1.7 million into five exceptional immunotherapy projects led by top prostate cancer research teams across the UK. Meet the team below.
Immunotherapy is an ingenious, effective treatment for many cancers. But it's had limited success in men with prostate cancer. Are we about to change that?
What is immunotherapy?
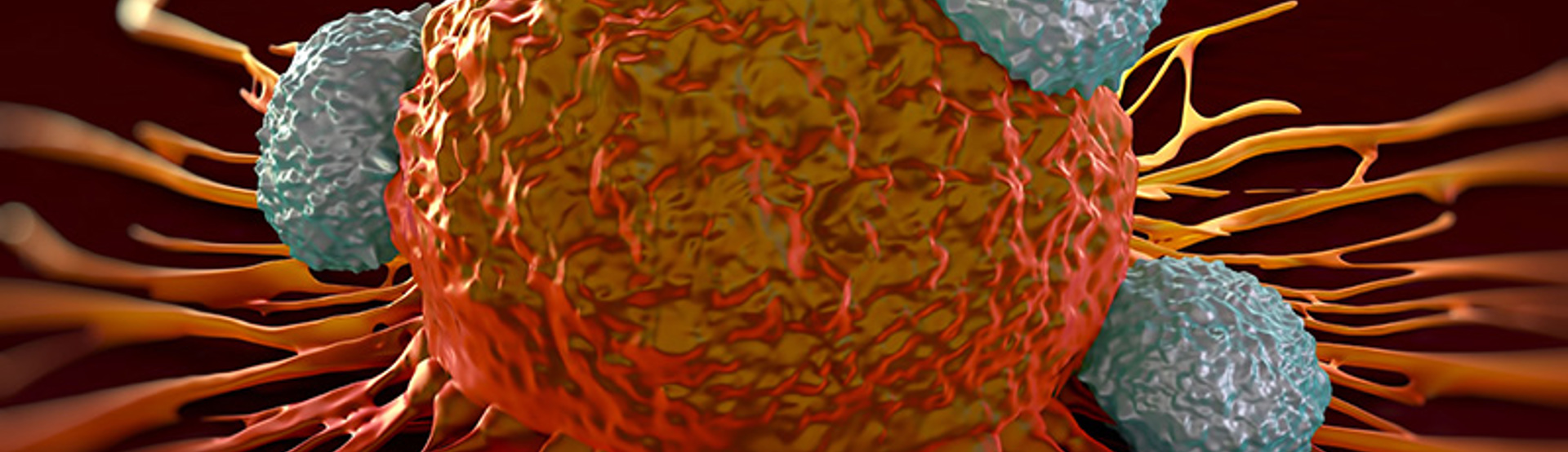
Immunotherapy treatments work by harnessing the power of your own immune system to treat cancer. With the help of these treatments, the immune cells can be trained to recognise intruding cancer cells and attack them.
Your immune system constantly patrols your body to detect and destroy any cells that are abnormal. This includes many early pre-cancerous cells. However, cancer cells will try to outwit the immune system by disguising themselves in a series of ways with genetic changes or surface proteins.
Simon Grieveson, our Head of Research, says: “Immunotherapy has revolutionised the treatment of many types of cancer, but so far this approach has only been successful in small numbers of men with prostate cancer. That’s why we’re investing in research to accelerate progress in this field and help develop more effective treatments for men diagnosed with prostate cancer. Funding innovative studies that tackle prostate cancer from new angles is vital to stop so many men dying from the disease.”
We caught up with researchers from three of these new projects to find out how their work could benefit men.

Combining targeted radiotherapy with immunotherapy for a double jolt to the immune system
Professor Katherine Vallis, University of Oxford
A promising new type of targeted radiotherapy treatment may soon become widely available for men with advanced prostate cancer, but we don’t fully understand its wider effects. The new drug called Lu-PSMA works to ‘seek and destroy’ cancer cells. One part of the drug attaches to a protein called a PSMA receptor, which is commonly produced by prostate cancer cells. This brings the cancer cells into close contact with the other part of the drug – a radioactive Lutetium-177 atom.
Lu-PSMA delivers radiation from inside the body. This can provide a more targeted treatment than aiming a beam of radiation from outside the body, as currently happens in conventional radiotherapy.
Recent research has suggested that traditional radiotherapy can stimulate the immune system to attack cancer cells. Now, Professor Vallis wants to see if Lu-PSMA can do the same, and whether this effect can be boosted by combining it with immunotherapy. . She said: “By analysing immune responses to the drug, we can see if it activates immune cells to kill prostate cancer, and if this helps stop the spread of the disease. The results will help us design clinical trials to test whether combining Lu-PSMA with other immune-boosting drugs enhances its cancer-fighting potential and maximises its benefits for men.”
"Immunotherapy has revolutionised the treatment of many types of cancer, but so far this approach has only been successful in small numbers of men with prostate cancer. Funding innovative studies that tackle prostate cancer from new angles is vital to stop so many men dying from the disease."
Simon Grieveson, Head of Research
Identifying the ‘STING in the tail’
Professor Richard Bryant and Dr Eileen Parkes, University of Oxford
About 1 in 6 cases of prostate cancer have a lot of inflammation in the surrounding area and this means they are more likely to spread and recur after treatment. Professor Richard Bryant and Dr Eileen Parkes believe that this may be due to triggering a chain of events in the cell known as the STING pathway.
Previous work by Professor Bryant and Dr Parkes found that prostate cancers which have activated the STING pathway have a lot of immune cells present. They believe that the STING pathway allows the cancer to hijack the immune system, so rather than working to destroy the cancer, the immune cells help it to grow more aggressively.
In this project, the team want to understand the role of the immune system in cases of prostate cancer with inflammation, particularly how the STING pathway responds to radiotherapy. If successful, this could lead to clinical trials of treatments that can be combined with radiotherapy to reduce the recurrence of prostate cancer.
Professor Bryant said: “Radiotherapy is an effective treatment for prostate cancer, but early evidence suggests it causes an immune response that helps make any surviving cancer cells more aggressive and likely to spread.”
Dr Parkes said: “By understanding how radiotherapy triggers prostate cancer to hijack the immune system in this way, we hope to find treatments that can stop this from happening and reduce the chances of the cancer returning.”

Developing a blood test that could show who will benefit from immunotherapy
Professor Aled Clayton, University of Cardiff
Though immunotherapy is an exciting field with huge amounts of potential, immunotherapies currently only work in rare cases for prostate cancer and it’s not clear why. Professor Aled Clayton at the University of Cardiff seeks to understand why some men benefit from these treatments, but others don’t. He believes that the way prostate cancer changes its surrounding environment may affect the immune system response.
Previous work from Professor Clayton has shown that prostate cancer tumours release small packages of molecules into the bloodstream, which can stop immune cells from working. As part of this project, the team will develop new methods to identify these packages in the blood.
Professor Clayton said: “This project will ultimately help us design approaches to treat prostate cancer by making immunotherapy a more effective and predictable treatment. In the future, we hope this could lead to blood tests which could check whether a particular form of immunotherapy is likely to work or not. This would help to ensure men are receiving the best possible treatment for their cancer.”
What could this mean for men with prostate cancer?
These projects could result in more treatment options for men with prostate cancer, as well as give us a better understanding of who will benefit from each treatment in advance. Although this is a complex area,it’s important to remember each cancer is as unique as each man.
Simon Grieveson, our Head of Research, reminds us: “Prostate cancer kills one man every 45 minutes in the UK. We desperately need better tests and treatments that will improve outcomes for men and give them valuable extra time with their loved ones. That’s why we’re proud to be funding innovative projects like these that will accelerate our knowledge and understanding of prostate cancer and take us one step closer to beating this devastating disease. We look forward to seeing how the projects develop over the next few years and the difference it will make to men’s lives”
Will you help unlock immunotherapy for men?
Funding varied research is essential to get the most from this promising branch of treatment. Help us harness the power of the immune system and transform care for men. Give a one-off or regular gift today.


