If your prostate cancer comes back
What is recurrent prostate cancer?
Recurrent prostate cancer is when your cancer comes back after you’ve had a treatment that aimed to cure it. It's sometimes called prostate cancer recurrence or prostate cancer relapse.
Treatments that you might have had include:
- surgery (radical prostatectomy)
- external beam radiotherapy (EBRT)
- permanent seed brachytherapy
- high dose-rate brachytherapy
- high intensity focused ultrasound (HIFU)
- cryotherapy
All these treatments aim to get rid of the prostate cancer. But sometimes not all the cancer is successfully treated, or the cancer may have been more advanced than first thought.
Finding out your cancer has returned
It can be very difficult to learn that your cancer has come back. All the thoughts and feelings you had when you were first diagnosed can come back again and they may be even stronger than before.
It's normal to feel shocked, angry, frustrated, disappointed, worried or sad. All these are very normal ways to feel. Things can get easier over time but some of these feelings may stay with you. Lots of men find it helpful to talk to someone about their feelings. This might be a friend or family member or someone who is trained to listen, like a counsellor or your doctor or nurse. You can also talk to our Specialist Nurses or someone who’s been there through our one-to-one support service or online community.
For many men, prostate cancer is slow-growing, even when it comes back after treatment. Lots of men with recurrent prostate cancer continue to live long and active lives.
How do I know if my prostate cancer has come back?
Your doctors and nurses will have monitored you after your first treatment to check for any signs that the cancer has come back.
Usually the first sign that your cancer is starting to return is a continuous rise in the level of prostate specific antigen (PSA) in your blood. The PSA test is a very effective way of checking how successful your treatment has been. It can't show for certain if prostate cancer has come back, or where it might be. But it can be a useful sign that the cancer may have come back. The exact change in PSA level that suggests your cancer has come back depends on which treatment you had. Read more about PSA levels after different treatments.
Your doctor may do other tests to check if, and where, your cancer has come back. These may include a CT (computer tomography), MRI (magnetic resonance imaging), bone, or PET (positron emission tomography) scan. Read more about follow-up after treatment for prostate cancer.
What symptoms should I look out for?
If your cancer does come back, the first sign is likely to be a rise in your PSA level, rather than any symptoms.
However, it’s important to let your doctor or nurse know if you do get any new symptoms or side effects, or are worried that your cancer might have come back. Advanced prostate cancer (cancer that has spread from the prostate to other parts of the body) can cause symptoms, such as extreme tiredness (fatigue), bone pain and problems urinating. Physical problems will often be side effects of treatment rather than a sign that your cancer has come back.
Your doctor or nurse can help find out what might be causing your symptoms and help you manage any side effects. They can also look at your PSA level to see whether or not your cancer might have come back.
Why has my cancer come back?
It’s not always completely clear why prostate cancer comes back, but there are two main possible reasons.
- Not all of the cancer cells in your prostate were treated during your first treatment. Small groups of cells might have been left behind. Over time, these may have grown large enough to be picked up by tests or to cause symptoms.
- The cancer was more advanced than your doctor originally thought. Tests or scans you had when you were diagnosed might have missed small clusters of cancer cells outside your prostate, for example in your lymph nodes or bones (see the diagram below). Your first treatment would not have been aimed at these cells. Over time, these cells may have grown large enough to be picked up by tests or to cause symptoms.
When you were diagnosed, your doctor would not have been able to tell you whether or not your cancer would come back. But they may have said how likely it was. Read more about your chance of cancer coming back.
Where could my prostate cancer come back?
Your prostate cancer can have come back in one or more areas. It could be:
- in your prostate, if it hasn’t been removed by surgery
- in the area around where your prostate used to be (the prostate bed) if the prostate has been removed by surgery
- in the area just outside your prostate
- in other parts of your body.
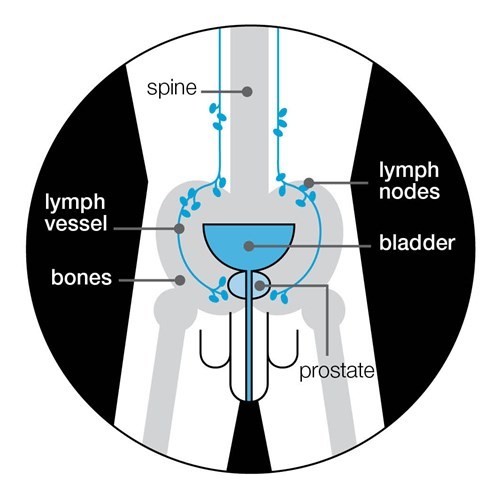
Prostate cancer can spread to any part of the body but it most commonly spreads to the bones and lymph nodes.
Prostate cancer that has spread to other parts of the body is known as advanced prostate cancer.
Sometimes it’s not clear where the cancer is. Some men may have a rise in their PSA level but the cancer may not show up on other tests, at least at first. This is quite common and your doctor will discuss treatment options with you.
What treatments are there for recurrent prostate cancer?
Treatments for recurrent prostate cancer are called second-line or salvage treatments. Many of the treatments used to treat prostate cancer when it’s first diagnosed can also be used as second-line treatments.
Making a decision about treatment
Your doctor might offer you one treatment, or a choice of treatments for recurrent prostate cancer. You may also be able to have your cancer monitored rather than treated straight away (see below). Or you might decide you don't want more treatment, other than treatment to help manage any symptoms you might get.
All treatments have advantages, disadvantages and side effects. Everyone is different and some side effects might be a problem for one man but not for another. It’s important to discuss your options with your doctor before deciding on a treatment. You could also talk through your options with your partner, family or friends, or speak to our Specialist Nurses.
What second-line treatments are there?
There are two main types of treatments – those that aim to get rid of the cancer (curative treatments) and those that aim to delay the cancer growing but won’t get rid of it.
Treatments aiming to get rid of the cancer
- External beam radiotherapy uses high-energy X-ray beams to destroy cancer cells. You might have it with or without hormone therapy.
- Permanent seed brachytherapy involves implanting tiny radioactive seeds into your prostate.
- High dose-rate brachytherapy involves inserting thin tubes into the prostate. A source of radiation is passed down the tubes into the prostate for a few minutes. The tubes are then taken out.
- Surgery (radical prostatectomy) removes your prostate and the cancer inside it.
- High intensity focused ultrasound (HIFU) uses ultrasound waves to heat and destroy cancer cells in your prostate. HIFU is newer than some other treatments, so isn’t available everywhere.
- Cryotherapy uses extreme cold to freeze and destroy cancer cells. It's newer than other treatments, so isn't available everywhere.
Treatments aiming to control the cancer
- Hormone therapy works by either lowering the amount of testosterone in the body or by stopping it from reaching the cancer cells, wherever they are in the body. Prostate cancer cells usually need testosterone to grow.
- Chemotherapy uses anti-cancer drugs to kill cancer cells, wherever they are in the body. You may be offered chemotherapy alongside hormone therapy. It can cause some serious side effects so you will need to be fit enough to cope with these.
Some men who have recurrent prostate cancer decide to take part in clinical trials of new treatments or new combinations of existing treatments. If you are interested in taking part in a clinical trial, ask your doctor if there are any that would be suitable for you.
Monitoring your prostate cancer
You may be able to have your cancer monitored, instead of having second-line treatment straight away. For many men, prostate cancer is slow-growing and may not cause any problems or symptoms, even without treatment. The aim of monitoring is to avoid or delay treatment, and the side effects that treatment can cause.
If you decide not to have treatment straight away, your doctor and nurse will monitor you and your cancer closely for any changes. You'll have regular PSA tests. You may also have other tests and scans.
If the tests show that your cancer is growing more quickly than expected, or if you have symptoms, talk to your doctor about starting second-line treatment.
Which second-line treatments are available to me?
It’s unlikely that all of the treatments will be available to you. Several things affect which treatments are suitable, including:
- where your cancer is
- your general health
- your PSA level and other test results
- what treatment you’ve already had.
Where your cancer is
Cancer that has returned in the prostate or the prostate bed is called local recurrence. If you have local recurrence, you might be offered further treatment aiming to get rid of the cancer.
Cancer that has spread to the area just outside the prostate, but not to other parts of the body, is called locally advanced recurrence. Some men with locally advanced recurrence will also be offered treatment that aims to get rid of the cancer.
But if your cancer has spread to other parts of your body (advanced prostate cancer), then treatment can no longer cure it. You will be offered hormone therapy to control the cancer, rather than getting rid of it. You might also be offered chemotherapy alongside hormone therapy.
Your general health
Your health and any other medical problems will also affect what treatments are available to you. For example, you may already have side effects from the first treatment you had. Having another treatment can cause side effects as well, so you’ll need to be fit enough to cope with this.
Your PSA level and other test results
Your PSA level and how fast it is rising will affect what treatments you are offered. You might have the option of monitoring your PSA level for a while before you have further treatment, particularly if your PSA level is rising slowly. If your PSA level is rising quickly, this suggests your cancer is more likely to have spread further.
What treatment you've already had
If your first treatment was surgery (radical prostatectomy), you might be able to have:
- radiotherapy to the prostate bed (with or without hormone therapy)
- hormone therapy alone.
If your first treatment was external beam radiotherapy, you might be able to have:
- hormone therapy
- HIFU (high-intensity focused ultrasound)
- cryotherapy
- brachytherapy
- surgery
If your first treatment was permanent seed brachytherapy or high dose-rate brachytherapy, you might be able to have:
- hormone therapy
- external beam radiotherapy
- more brachytherapy
- surgery
- cryotherapy
- HIFU, but this is rare and not available everywhere.
If your first treatment was HIFU (high-intensity focused ultrasound), you might be able to have:
- more HIFU
- external beam radiotherapy
- cryotherapy
- hormone therapy
- surgery, but this is rare.
If your first treatment was cryotherapy, you might be able to have:
- more cryotherapy
- HIFU
- external beam radiotherapy
- hormone therapy
- surgery, but this is rare
Speak to your doctor or nurse about which treatments are available to you.
Side effects of second-line treatment
All treatments have side effects. The risk of side effects is usually higher when a treatment is used as a second-line treatment than when it’s used as your first treatment. This is because your first treatment may have already caused some damage to the tissue surrounding the prostate.
Side effects may also be more severe with a second-line treatment. And you might still be getting side effects from your first treatment.
Ask your doctor or nurse for more information about the possible side effects from the second-line treatments they offer you. Read our treatment pages to find out about side effects from different treatments. Finding out about possible side effects might help you to choose between your different treatment options, or whether you want to have any treatment.
What if I don't want further treatment?
Some men weigh up the advantages and disadvantages and decide they don't want to have second-line treatment for their cancer. Speak to your doctor or nurse if you are thinking about not having further treatment. They may suggest observing your prostate cancer with regular tests. If it starts to cause symptoms then you’re likely to be offered hormone therapy to control the cancer and help relieve symptoms. There are also other treatments to manage symptoms.
When will my treatment start?
This varies from man to man. For example, your doctor might want to delay it if you are still recovering from the side effects of your first treatment. Ask your doctor or nurse for more information about when your treatment will start.
If you have treatment that aims to get rid of the cancer
If you’re having treatment that aims to get rid of the cancer, your treatment could start straight away. But for some men, there might be an option to delay treatment until tests show that the cancer is growing more quickly.
If you have treatment that aims to control your cancer
If you’re having hormone therapy to control your cancer, when you start treatment will depend on several things, including:
- whether your prostate cancer has spread to other parts of your body
- whether you have any symptoms from your cancer
- how quickly your PSA level is rising
- how you feel about starting treatment.
You might start hormone therapy straight away or you might be monitored for a while before you start. Monitoring involves regular check-ups and PSA tests. If your PSA reaches a level that suggests your cancer is growing more quickly, you will then be offered hormone therapy.
Some men feel uneasy knowing that their cancer is back and isn’t being treated, but there can be good reasons to delay hormone therapy. These include:
- if you still have side effects from your first treatment
- to delay having side effects of hormone therapy, such as sexual problems, hot flushes and fatigue.
If you are on life-long hormone therapy and having problems with side effects, you might be able to have intermittent hormone therapy.
Read more about hormone therapy and its side effects. If you are concerned about delaying the start of treatment, discuss this with your doctor or nurse.
What happens after second-line treatment?
You will have regular follow-up appointments to monitor how well your treatment is working. The aim is to:
- check how your cancer has responded to treatment
- deal with any side effects of treatment
- give you a chance to raise any concerns or ask any questions.
You will have regular PSA tests as part of this follow-up. Read more about what to expect from your follow-up care.
What if my cancer comes back again?
If your cancer comes back again after treatment that aimed to get rid of it, you will be offered hormone therapy to control your cancer, though you may not need to start it straight away.
Hormone therapy can keep your cancer under control for many months or years before you need to think about other treatments.
But over time, your cancer may start to grow again. You may continue having your original hormone therapy, but there are also other treatments available. Read more about treatment options after your first hormone therapy.
Some men decide they would like to take part in a clinical trial of a new treatment or a new combination of existing treatments.
What if I develop symptoms?
Tell your doctor or nurse about any symptoms you have. If you have symptoms between your check-ups, tell your doctor or nurse as soon as possible. If these are signs of the cancer coming back, they can talk to you about treatment options.
Your doctor or nurse can also give you advice and treatment to help manage your symptoms. For example, if your cancer has spread to the bones and is causing pain, there are treatments to help, such as pain-relieving medication, drugs called bisphosphonates and pain-relieving radiotherapy.
Dealing with recurrent prostate cancer
A lot of men find it hard if they discover their cancer has come back. All the emotions you had when you were first diagnosed can resurface and they may be even stronger the second time round.
Some men feel angry that their cancer has come back. It is normal to want to find an explanation, but remember it’s not your fault – try to go easy on yourself.
The thought of more treatment can be overwhelming. You may feel less hopeful than you did before. However, men do have successful treatment for recurrent prostate cancer.
You may also have practical concerns about your cancer coming back, for example, worries about work or money.
Read more about living with or after prostate cancer and what can help.
References
Updated: March 2023 | Due for review: April 2024
- Ahmed HU, Ishaq A, Zacharakis E, Shaw G, Illing R, Allen C, et al. Rectal fistulae after salvage high-intensity focused ultrasound for recurrent prostate cancer after combined brachytherapy and external beam radiotherapy. BJU Int. 2009 Feb;103(3):321–3.
- Allan CA, Collins VR, Frydenberg M, McLachlan RI, Matthiesson KL. Androgen deprivation therapy complications. Endocr Relat Cancer. 2014 Jul 22;21(4):T119–29.
- Allott EH, Masko EM, Freedland SJ. Obesity and Prostate Cancer: Weighing the Evidence. Eur Urol. 2013 May;63(5):800–9.
- Autran-Gomez AM, Scarpa RM, Chin J. High-Intensity Focused Ultrasound and Cryotherapy as Salvage Treatment in Local Radio-Recurrent Prostate Cancer. Urol Int. 2012;89(4):373–9.
- Baumann FT, Zopf EM, Bloch W. Clinical exercise interventions in prostate cancer patients: a systematic review of randomized controlled trials. Support Care Cancer. 2012;20(2):221–33.
- Botrel TEA, Clark O, dos Reis RB, Pompeo ACL, Ferreira U, Sadi MV, et al. Intermittent versus continuous androgen deprivation for locally advanced, recurrent or metastatic prostate cancer: a systematic review and meta-analysis. BMC Urol. 2014;14:9.
- Botrel TEA, Clark O, Lima Pompeo AC, Horta Bretas FF, Sadi MV, Ferreira U, et al. Efficacy and Safety of Combined Androgen Deprivation Therapy (ADT) and Docetaxel Compared with ADT Alone for Metastatic Hormone-Naive Prostate Cancer: A Systematic Review and Meta-Analysis. PLoS ONE [Internet]. 2016 Jun 16 [cited 2018 Oct 29];11(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4911003/
- Bourke L, Smith D, Steed L, Hooper R, Carter A, Catto J, et al. Exercise for Men with Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol. 2016 Apr;69(4):693–703.
- Cao Y, Ma J. Body Mass Index, Prostate Cancer-Specific Mortality, and Biochemical Recurrence: a Systematic Review and Meta-analysis. Cancer Prev Res (Phila Pa). 2011 Jan 13;4(4):486–501.
- Chade DC, Eastham J, Graefen M, Hu JC, Karnes RJ, Klotz L, et al. Cancer Control and Functional Outcomes of Salvage Radical Prostatectomy for Radiation-recurrent Prostate Cancer: A Systematic Review of the Literature. Eur Urol. 2012 May;61(5):961–71.
- Cormie P, Galvão DA, Spry N, Joseph D, Chee R, Taaffe DR, et al. Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: a randomised controlled trial. BJU Int. 2015;115(2):256–66.
- Darcey E, Boyle T. Tobacco smoking and survival after a prostate cancer diagnosis: A systematic review and meta-analysis. Cancer Treat Rev. 2018 Nov;70:30–40.
- Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer. 2011 Nov 8;105:S52–73.
- De Nunzio C, Andriole GL, Thompson IM, Freedland SJ. Smoking and Prostate Cancer: A Systematic Review. Eur Urol Focus. 2015 Aug;1(1):28–38.
- Discacciati A, Orsini N, Wolk A. Body mass index and incidence of localized and advanced prostate cancer--a dose-response meta-analysis of prospective studies. Ann Oncol. 2012 Jan 6;23(7):1665–71.
- Foerster B, Pozo C, Abufaraj M, Mari A, Kimura S, D’Andrea D, et al. Association of Smoking Status With Recurrence, Metastasis, and Mortality Among Patients With Localized Prostate Cancer Undergoing Prostatectomy or Radiotherapy: A Systematic Review and Meta-analysis. JAMA Oncol [Internet]. 2018 May 24 [cited 2018 May 29]; Available from: http://oncology.jamanetwork.com/article.aspx?doi=10.1001/jamaoncol.2018.1071
- Gandaglia G, Briganti A, Clarke N, Karnes RJ, Graefen M, Ost P, et al. Adjuvant and Salvage Radiotherapy after Radical Prostatectomy in Prostate Cancer Patients. Eur Urol. 2017 Nov;72(5):689–709.
- Gardner JR, Livingston PM, Fraser SF. Effects of Exercise on Treatment-Related Adverse Effects for Patients With Prostate Cancer Receiving Androgen-Deprivation Therapy: A Systematic Review. J Clin Oncol. 2014 Feb 1;32(4):335–46.
- Gerdtsson A, Poon JB, Thorek DL, Mucci LA, Evans MJ, Scardino P, et al. Anthropometric Measures at Multiple Times Throughout Life and Prostate Cancer Diagnosis, Metastasis, and Death. Eur Urol. 2015 Dec;68(6):1076–82.
- Gomez-Veiga F, Mariño A, Alvarez L, Rodriguez I, Fernandez C, Pertega S, et al. Brachytherapy for the treatment of recurrent prostate cancer after radiotherapy or radical prostatectomy. BJU Int. 2012;109(s1):17–21.
- Grossmann M, Hamilton EJ, Gilfillan C, Bolton D, Joon DL, Zajac JD. Bone and metabolic health in patients with non-metastatic prostate cancer who are receiving androgen deprivation therapy. Med J Aust. 2011;194(6):301–6.
- Hannan JL, Maio MT, Komolova M, Adams MA. Beneficial Impact of Exercise and Obesity Interventions on Erectile Function and Its Risk Factors. J Sex Med. 2009 Mar;6(S3):254–61.
- Hechtman LM. Clinical Naturopathic Medicine [Internet]. Harcourt Publishers Group (Australia); 2014 [cited 2015 Jul 21]. 1610 p. Available from: http://www.bookdepository.com/Clinical-Naturopathic-Medicine-Leah-Hechtman/9780729541923
- Henson CC, Burden S, Davidson SE, Lal S. Nutritional interventions for reducing gastrointestinal toxicity in adults undergoing radical pelvic radiotherapy. Cochrane Database Syst Rev [Internet]. 2013 [cited 2014 Nov 18];(11). Available from: http://doi.wiley.com/10.1002/14651858.CD009896.pub2
- Ho T, Gerber L, Aronson WJ, Terris MK, Presti JC, Kane CJ, et al. Obesity, Prostate-Specific Antigen Nadir, and Biochemical Recurrence After Radical Prostatectomy: Biology or Technique? Results from the SEARCH Database. Eur Urol. 2012 Nov;62(5):910–6.
- Hu MB, Xu H, Bai PD, Jiang HW, Ding Q. Obesity has multifaceted impact on biochemical recurrence of prostate cancer: a dose-response meta-analysis of 36,927 patients. Med Oncol Northwood Lond Engl. 2014 Feb;31(2):829.
- Huncharek M, Haddock KS, Reid R, Kupelnick B. Smoking as a risk factor for prostate cancer: a meta-analysis of 24 prospective cohort studies. J Inf. 2010;100(4).
- Husson O, Mols F, Poll-Franse LV van de. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Ann Oncol. 2010 Sep 24;mdq413.
- Islami F, Moreira DM, Boffetta P, Freedland SJ. A Systematic Review and Meta-analysis of Tobacco Use and Prostate Cancer Mortality and Incidence in Prospective Cohort Studies. Eur Urol. 2014 Dec;66(6):1054–64.
- Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, et al. Effects of resistance exercise in prostate cancer patients: a meta-analysis. Support Care Cancer. 2017 Jun 10;
- Kenfield SA, Stampfer MJ, Chan JM, Giovannucci E. Smoking and prostate cancer survival and recurrence. JAMA. 2011;305(24):2548.
- Keogh JWL, MacLeod RD. Body Composition, Physical Fitness, Functional Performance, Quality of Life, and Fatigue Benefits of Exercise for Prostate Cancer Patients: A Systematic Review. J Pain Symptom Manage. 2012 Jan;43(1):96–110.
- Keto CJ, Aronson WJ, Terris MK, Presti JC, Kane CJ, Amling CL, et al. Obesity is associated with castration-resistant disease and metastasis in men treated with androgen deprivation therapy after radical prostatectomy: results from the SEARCH database. BJU Int. 2011;110(4):492–8.
- Kimura M, Mouraviev V, Tsivian M, Mayes JM, Satoh T, Polascik TJ. Current salvage methods for recurrent prostate cancer after failure of primary radiotherapy. BJU Int. 2010 Jan;105(2):191–201.
- Larkin D, Lopez V, Aromataris E. Managing cancer-related fatigue in men with prostate cancer: A systematic review of non-pharmacological interventions. Int J Nurs Pract. 2014 Oct;20(5):549–60.
- Lawrentschuk N, Finelli A, Van der Kwast TH, Ryan P, Bolton DM, Fleshner NE, et al. Salvage Radical Prostatectomy Following Primary High Intensity Focused Ultrasound for Treatment of Prostate Cancer. J Urol. 2011 Mar;185(3):862–8.
- Lin PH, Aronson W, Freedland SJ. Nutrition, dietary interventions and prostate cancer: the latest evidence. BMC Med. 2015 Jan 8;13:3.
- Magnan S, Zarychanski R, Pilote L, Bernier L, Shemilt M, Vigneault E, et al. Intermittent vs Continuous Androgen Deprivation Therapy for Prostate Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2015 Sep 17;1–10.
- Meldrum DR, Gambone JC, Morris MA, Esposito K, Giugliano D, Ignarro LJ. Lifestyle and metabolic approaches to maximizing erectile and vascular health. Int J Impot Res. 2012 Apr;24(2):61–8.
- Mendenhall WM, Henderson RH, Hoppe BS, Nichols RC, Mendenhall NP. Salvage of Locally Recurrent Prostate Cancer After Definitive Radiotherapy: Am J Clin Oncol. 2014 Aug;37(4):411–6.
- Menichetti J, Villa S, Magnani T, Avuzzi B, Bosetti D, Marenghi C, et al. Lifestyle interventions to improve the quality of life of men with prostate cancer: A systematic review of randomized controlled trials. Crit Rev Oncol Hematol. 2016 Dec;108:13–22.
- Mohamad H, McNeill G, Haseen F, N’Dow J, Craig LCA, Heys SD. The Effect of Dietary and Exercise Interventions on Body Weight in Prostate Cancer Patients: A Systematic Review. Nutr Cancer. 2015 Jan 2;67(1):43–60.
- Mottet et al. EAU Guidelines on Prostate Cancer [Internet]. [cited 2023 Mar 20]. Available from: https://uroweb.org/guidelines/prostate-cancer
- Mydin AR, Dunne MT, Finn MA, Armstrong JG. Early Salvage Hormonal Therapy for Biochemical Failure Improved Survival in Prostate Cancer Patients After Neoadjuvant Hormonal Therapy Plus Radiation Therapy—A Secondary Analysis of Irish Clinical Oncology Research Group 97-01. Int J Radiat Oncol. 2013 Jan;85(1):101–8.
- National Institute for Clinical Excellence. High-intensity focused ultrasound for prostate cancer. Interventional procedure guidance 118. 2005.
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management [Internet]. 2021 [cited 2022 Dec 19]. Available from: https://www.nice.org.uk/guidance/ng131
- National Institute for Health and Clinical Excellence. Cryotherapy for recurrent prostate cancer. Interventional procedure guidance 119. 2005.
- National Institute for Health and Clinical Excellence. Focal therapy using high-intensity focused ultrasound for localised prostate cancer. NICE interventional procedure guidance 424. 2012.
- Parekh A, Graham PL, Nguyen PL. Cancer Control and Complications of Salvage Local Therapy After Failure of Radiotherapy for Prostate Cancer: A Systematic Review. Semin Radiat Oncol. 2013 Jul;23(3):222–34.
- Pettersson A, Johansson B, Persson C, Berglund A, Turesson I. Effects of a dietary intervention on acute gastrointestinal side effects and other aspects of health-related quality of life: A randomized controlled trial in prostate cancer patients undergoing radiotherapy. Radiother Oncol. 2012 Jun;103(3):333–40.
- Pfister D, Bolla M, Briganti A, Carroll P, Cozzarini C, Joniau S, et al. Early Salvage Radiotherapy Following Radical Prostatectomy. Eur Urol. 2014 Jun;65(6):1034–43.
- Punnen S, Cooperberg MR, D’Amico AV, Karakiewicz PI, Moul JW, Scher HI, et al. Management of Biochemical Recurrence After Primary Treatment of Prostate Cancer: A Systematic Review of the Literature. Eur Urol. 2013 Dec 1;64(6):905–15.
- Richman EL, Kenfield SA, Stampfer MJ, Paciorek A, Carroll PR, Chan JM. Physical Activity after Diagnosis and Risk of Prostate Cancer Progression: Data from the Cancer of the Prostate Strategic Urologic Research Endeavor. Cancer Res. 2011 May 24;71(11):3889–95.
- Rieken M, Shariat SF, Kluth LA, Fajkovic H, Rink M, Karakiewicz PI, et al. Association of Cigarette Smoking and Smoking Cessation with Biochemical Recurrence of Prostate Cancer in Patients Treated with Radical Prostatectomy. Eur Urol. 2015 Dec;68(6):949–56.
- Rohrmann S, Linseisen J, Allen N, Bueno-de-Mesquita HB, Johnsen NF, Tjønneland A, et al. Smoking and the risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition. Br J Cancer. 2013;108(3):708–14.
- Rosoff JS, Savage SJ, Prasad SM. Salvage radical prostatectomy as management of locally recurrent prostate cancer: outcomes and complications. World J Urol. 2013 Dec;31(6):1347–52.
- Sathianathen NJ, Butaney M, Konety BR. The utility of PET-based imaging for prostate cancer biochemical recurrence: a systematic review and meta-analysis. World J Urol [Internet]. 2018 Jul 12 [cited 2019 Feb 22]; Available from: http://link.springer.com/10.1007/s00345-018-2403-7
- Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without Antiandrogen Therapy in Recurrent Prostate Cancer. N Engl J Med. 2017 Feb 2;376(5):417–28.
- Silva FC da, Silva FMC da, Gonçalves F, Santos A, Kliment J, Whelan P, et al. Locally Advanced and Metastatic Prostate Cancer Treated with Intermittent Androgen Monotherapy or Maximal Androgen Blockade: Results from a Randomised Phase 3 Study by the South European Uroncological Group. Eur Urol. 2014 Aug;66(2):232–9.
- Solanki AA, Liauw SL. Tobacco use and external beam radiation therapy for prostate cancer: Influence on biochemical control and late toxicity. Cancer. 2013;n/a-n/a.
- Spratt DE, Dess RT, Zumsteg ZS, Lin DW, Tran PT, Morgan TM, et al. A Systematic Review and Framework for the Use of Hormone Therapy with Salvage Radiation Therapy for Recurrent Prostate Cancer. Eur Urol. 2018 Feb 1;73(2):156–65.
- Spratt DE, McHugh DJ, Morris MJ, Morgans AK. Management of Biochemically Recurrent Prostate Cancer: Ensuring the Right Treatment of the Right Patient at the Right Time. Am Soc Clin Oncol Educ Book. 2018 May 23;(38):355–62.
- Teleni L, Chan RJ, Chan A, Isenring EA, Vela I, Inder WJ, et al. Exercise improves quality of life in androgen deprivation therapy-treated prostate cancer: systematic review of randomised controlled trials. Endocr Relat Cancer. 2016 Jan 2;23(2):101–12.
- Thong MSY, Mols F, Coebergh JWW, Roukema JA, van de Poll-Franse LV. The impact of disease progression on perceived health status and quality of life of long-term cancer survivors. J Cancer Surviv. 2009 Sep;3(3):164–73.
- Tillisch K. Complementary and alternative medicine for functional gastrointestinal disorders. Gut. 2006 May 1;55(5):593–6.
- Ullrich PM, Carson MR, Lutgendorf SK, Williams RD. Cancer Fear and Mood Disturbance After Radical Prostatectomy: Consequences of Biochemical Evidence of Recurrence. J Urol. 2003 Apr;169(4):1449–52.
- van den Bergh RCN, van Casteren NJ, van den Broeck T, Fordyce ER, Gietzmann WKM, Stewart F, et al. Role of Hormonal Treatment in Prostate Cancer Patients with Nonmetastatic Disease Recurrence After Local Curative Treatment: A Systematic Review. Eur Urol. 2016 May;69(5):802–20.
- Van den Broeck T, van den Bergh RCN, Arfi N, Gross T, Moris L, Briers E, et al. Prognostic Value of Biochemical Recurrence Following Treatment with Curative Intent for Prostate Cancer: A Systematic Review. Eur Urol [Internet]. 2018 Oct [cited 2019 Feb 22]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S0302283818307528
- Wang LS, Murphy CT, Ruth K, Zaorsky NG, Smaldone MC, Sobczak ML, et al. Impact of obesity on outcomes after definitive dose-escalated intensity-modulated radiotherapy for localized prostate cancer. Cancer. 2015 Sep 1;121(17):3010–7.
- Wedlake LJ, Shaw C, Whelan K, Andreyev HJN. Systematic review: the efficacy of nutritional interventions to counteract acute gastrointestinal toxicity during therapeutic pelvic radiotherapy. Aliment Pharmacol Ther. 2013 Jun;37(11):1046–56.
- Wolin KY, Luly J, Sutcliffe S, Andriole GL, Kibel AS. Risk of Urinary Incontinence Following Prostatectomy: The Role of Physical Activity and Obesity. J Urol. 2010 Feb;183(2):629–33.
- World Cancer Research Fund International. Continuous Update Project report: Diet, Nutrition, Physical Activity and Prostate Cancer [Internet]. 2014. Available from: www.wcrf.org/sites/default/files/Prostate-Cancer-2014-Report.pdf
- Zu K, Giovannucci E. Smoking and aggressive prostate cancer: a review of the epidemiologic evidence. Cancer Causes Control. 2009 Jun 27;20(10):1799–810.
