Urinary problems after prostate cancer treatment
Many men get urinary problems as a side effect of their treatment. This is because prostate cancer treatment can damage the nerves and muscles that control when you urinate (wee).
If you’re starting treatment for prostate cancer, ask your doctor about the possible side effects. Each treatment can cause different urinary problems. Your chances of getting each side effect will depend on the treatment you’re having, and on whether or not you had urinary problems before starting treatment.
If you’ve already had prostate cancer treatment and you have urinary problems, tell your doctor or nurse. They can suggest treatments and lifestyle changes to help manage them.
Depending on the type of problems you’re having, ways to manage them can include lifestyle changes, pelvic floor muscle exercises, bladder retraining, medicines or surgery.
Watch Paul's story below for one man's experience of managing urinary problems after prostate cancer treatment.

Urinary problems after prostate cancer treatment fact sheet
This fact sheet is for anyone who wants to know more about urinary problems after treatment for prostate cancer.
Problems after surgery (radical prostatectomy)
Surgery can cause urinary problems, including:
- leaking urine
- difficulty urinating.
Leaking urine
This is the most common urinary problem after surgery. When you wake up after surgery, you’ll have a thin tube called a catheter in your body. This is to drain urine out of your body. You’ll usually have a catheter for about seven to ten days after surgery.
Most men can’t control their bladder properly when their catheter is first removed. This is because surgery can damage the muscles and nerves that control when you urinate, including the urinary sphincter and the pelvic floor muscles. Recovering from this damage can take some time.
Your hospital may give you some absorbent incontinence pads to put in your underwear. But you might want to take some pads, and a spare pair of pants and trousers with you when you go to have your catheter removed. Close fitting underwear can help to keep the pads in place, and men often find loose, lightweight trousers most comfortable.
You might just leak a few drops when you exercise, cough or sneeze (stress incontinence). Or you might leak larger amounts. Some men also leak urine when they get an erection or during sex. This isn’t harmful as urine is usually germ-free, but it might bother you or your partner.
If I went to stretch for something, or got out the shower and there was a change of temperature, or if I coughed, I would leak.
What can help with leaking urine?
There are treatments and products available that can help, and there are things you can do to help yourself. Your treatment options will depend on how much urine you’re leaking, and how recently you had your prostate cancer treatment.
Treatments and products available that can help include:
- absorbent pads and pants
- pelvic floor muscle exercises
- urinary sheaths
- bed protectors and handheld urinals
- penile clamps.
If you have sudden urges to urinate (urinary urgency) and sometimes leak urine before you get to the toilet (urge incontinence), you may be offered bladder retraining.
If you still leak urine six to twelve months after surgery and pelvic floor muscle exercises haven’t helped, there are treatments available that might help. These may include:
- an internal male sling
- an artificial urinary sphincter
- adjustable balloons
- medicines.
Talk to your doctor or nurse about treatments and products that may be suitable for you.
Absorbent pads and pants
These can be worn inside your underwear or instead of underwear to soak up any leaks. Some people find it helpful to wear close fitting underwear with pads. You may want to try female pads as your leaking improves, as these tend to be smaller and lighter and may fit better. Pads are usually very discreet, so people won’t know you’re wearing them. But you may feel more confident wearing dark trousers so it won’t show as much if your pad does leak.
Can I get my products for free?
Services vary from area to area, but your GP or the continence nurses at your hospital may provide some pads for free. Or you can buy them in supermarkets, chemists or online. Age UK also has a range of products that can be ordered online.
If you haven’t had your operation yet, you might find it helps to prepare by finding out what products are available. Talk to your doctor, nurse or continence advisor for more information, or visit the Continence Product Advisor website.
Pelvic floor muscle exercises
These can strengthen the pelvic floor muscles, which help control when you urinate.
Read about pelvic floor muscle exercises.
Urinary sheaths
You might hear these called external catheters. These look like condoms with a tube attached to the end that drains urine into a bag. The sheath fits tightly over the penis and you can strap the bag to your leg – under your clothes – and empty it as needed.
Bed protectors and handheld urinals
If you have to go to the toilet often during the night, or you leak urine when you’re in bed, bed protectors or handheld urinals might be useful to you.
Bed protectors are large pads that protect your sheets and mattress by soaking up any urine that you might leak. There are pads that you can wash and reuse, and others that you only use once before throwing them away
Handheld urinals are containers with a lid that can be used if you can’t reach the toilet in time or if there isn’t a toilet nearby. They have a large opening with a lid so that you can store the urine until you reach a toilet. These might also be useful if you drive long distances and don’t have any toilet near you.
Penile clamps
A penile clamp fits onto the penis and squeezes it, closing the urethra so that no urine can leak out. You should only use a penile clamp during the day for short periods of time, and should open it at least every two hours to let your blood flow back into your penis.
A penile clamp fits onto the penis and squeezes it, closing the urethra so that no urine can leak out. You should only use a penile clamp during the day for short periods of time, and should open it at least every two hours to let your blood flow back into your penis.
Penile clamps can be uncomfortable to wear and aren’t commonly used in the UK. They aren’t usually recommended by health professionals, as they reduce the blood flow to the penis. This means it can be unsafe if a clamp is put on too tightly or for too long. However, some men like to use them for activities such as swimming or jogging.
For more information about the different types of products to manage leaking urine, visit Continence Product Advisor.
Internal male sling
This is a small piece of material (mesh) that presses gently on your urethra and supports the urinary sphincter to keep it closed. This helps to stop urine leaking. You’ll have an operation to fit the sling. It should be tight enough to stop urine leaking out, but loose enough to let you urinate when you want to.
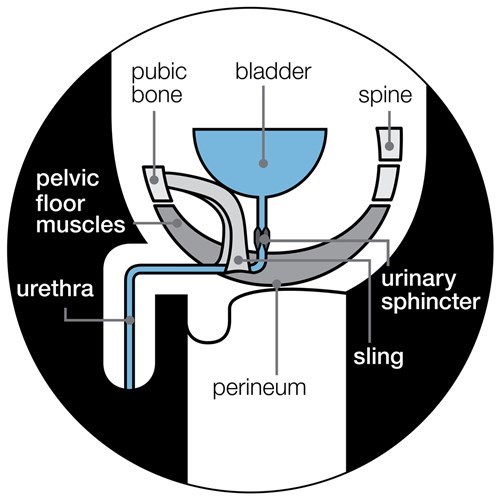
You may be able to have an internal sling if you still leak a mild to moderate amount of urine (if you use two to three pads a day) one year after your treatment for prostate cancer.
The sling may not work as well if you leak a lot of urine or have previously had radiotherapy.
You’ll have an operation to fit the internal sling. You will usually have a general anaesthetic so you’ll be asleep.
Like all treatments, there can be side effects.
- You may have some pain in the first three months after the operation.
- You might get an infection – about one in eight men may need their sling removed because of an infection.
- A small number of men have problems urinating (urine retention) after their operation, but this isn’t very common.
Your doctor or nurse can tell you more about the possible risks.
Artificial urinary sphincter
This involves surgery to fit a small device that consists of:
- a fluid-filled cuff that fits around your urethra
- a balloon in front of your bladder
- a pump in your scrotum (the skin around your testicles).
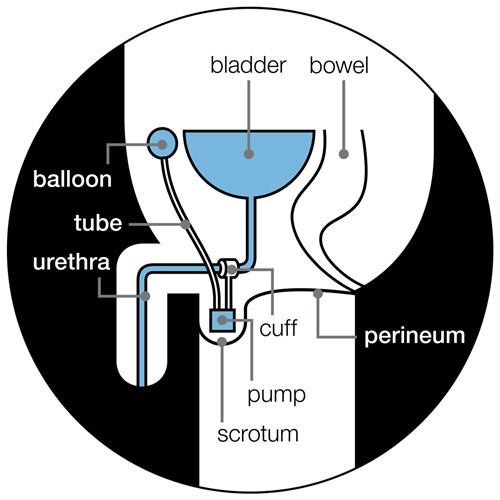
The cuff presses the urethra closed so that you don’t leak urine. This means you can control when you urinate.
- You squeeze the pump in your scrotum – this moves the fluid out of the cuff and into the balloon.
- When the cuff is empty it stops pressing your urethra closed, letting urine pass through the urethra so that you can urinate.
- After a few minutes, the fluid flows back into the cuff, pressing the urethra closed again.
An artificial urinary sphincter is usually only suitable for men who still leak a lot of urine at least six months after their prostate cancer treatment.
You’ll have an operation to fit the device. You will have a general anaesthetic, so you’ll be asleep and won’t feel anything.
Like all operations, there are risks in having an artificial urinary sphincter, such as infection or parts of the device breaking. This may be more likely if you’ve previously had radiotherapy. Some men need another operation to fix problems, and some may need to have their device removed. Your doctor or nurse can tell you more about the possible risks.
If your hospital doesn’t do this type of surgery, your doctor may be able to refer you to one that does.
Adjustable balloons
These consist of two small balloons that are placed around the urethra (the tube you urinate through). The fluid-filled balloons press on the urethra to stop urine leaking out – but you should still be able to urinate when you want to. A device called a ‘port’, which is placed in your scrotum allows your doctor to make the balloons bigger or smaller at any time.
Balloons aren’t common in the UK. But if your hospital doesn’t do this type of surgery, your doctor may be able to refer you to one that does. Balloons may be an option if you still leak urine more than six months after your prostate cancer treatment. But you probably won’t be able to have them if you’ve had radiotherapy.
Like all operations, there are risks in having adjustable balloons. They include infection, or the balloons shrinking or moving, and you may have to have the balloons removed. Your doctor or nurse can tell you more about the possible risks.
Medicines
If you continue to leak urine, or if other treatments aren’t suitable for you, you may be offered a medicine called an anti-cholinergic to help keep the urethra closed, or to calm your bladder down. This can help to reduce leakages. All drugs can cause side effects, so talk to your doctor or nurse about the possible side effects and how to manage them.
Difficulty urinating
Some men may find it difficult to urinate after surgery (urine retention). This is caused by scarring, which can cause the urethra to become narrow. This isn’t very common after surgery.
Problems after radiotherapy
Both external beam radiotherapy (EBRT) and brachytherapy can cause urinary problems, including:
- bladder irritation (radiation cystitis)
- needing to urinate more often (urinary frequency)
- a sudden urge to urinate (urinary urgency), and you may sometimes leak before you get to the toilet (urge incontinence)
- difficulty urinating (urine retention).
Some men may leak urine after radiotherapy, but this is less common. It is more likely if you’ve previously had an operation called a transurethral resection of the prostate (TURP) for an enlarged prostate.
Looking for information on bowel problems rather than urinary problems after prostate cancer treatment? Read more about bowel problems here.
Radiation cystitis
Radiotherapy can irritate the lining of the bladder and the urethra – this is called radiation cystitis. Symptoms include:
- needing to urinate more often, including at night
- a burning feeling when you urinate
- difficulty urinating
- blood in the urine.
Symptoms can start within a few days of your first treatment. They usually begin to improve when your treatment ends. But some men get symptoms for several months. And some don’t get symptoms until months or even years after their final treatment.
Symptoms such as blood in the urine can be worrying, but this is quite a common symptom of radiation cystitis.
If you get symptoms of radiation cystitis, tell your doctor or nurse. They can check whether your symptoms are caused by your treatment or an infection.
What can help with radiation cystitis?
There are treatments that can help with radiation cystitis, as well as things you can do yourself.
Lifestyle changes
Drink plenty of fluids (1.5-2 litres, or 3-4 pints a day), but try to avoid fizzy drinks, drinks containing caffeine – such as tea, coffee and cola – and alcohol, as these can irritate the bladder.
Although the evidence for this isn’t very strong, some men find that drinking cranberry juice helps. But you should avoid cranberry juice if you’re taking warfarin to thin your blood.
Bladder wash
If your symptoms are severe, your doctor may suggest a treatment called a bladder wash, such as Cystistat®. This is a liquid medicine that coats and protects the lining of the bladder, making it less irritated. A small tube (catheter) is passed up your penis and fills your bladder with the liquid medicine. You then go to the toilet to empty your bladder.
Urinary frequency and urgency
Some men find they need to urinate more often after having radiotherapy (frequency), or get a sudden urge that’s hard to ignore (urgency). You may also need to urinate more often at night (nocturia). It usually only lasts for a few months after radiotherapy, but if it happens, it might help to drink less in the two hours before you go to bed, and to avoid drinks that irritate the bladder
A small number of men leak urine before they can reach the toilet (urge incontinence). This happens when the bladder muscles twitch and squeeze (spasm) without you controlling them. This pushes urine out before you’re ready.
What can help with urinary frequency and urgency?
There are treatments that can help with urinary frequency and urgency, as well as things you can do yourself.
Bladder retraining
If you need to urinate more often than usual or sometimes leak before reaching the toilet, you could try a technique called bladder retraining. This can help you control when you urinate, and help you hold on for longer. Speak to your specialist continence nurse or physiotherapist for more information.
Medicines
Drugs called anti-cholinergics can help to reduce frequency, urgency and leaks. If you can't have anto-cholinergics, you may be offered mirabegron (Betmiga®) tablets.
Percutaneous posterior tibial nerve stimulation (PTNS)
This treatment may help some men to urinate and leak urine less often. A needle is placed under the skin just above your ankle. A low electrical current is passed through the needle to affect the nerves that control urination. This can help stop the bladder from emptying before it’s full.
You’ll normally have PTNS once a week for 12 weeks. Each treatment lasts about half an hour. PTNS has no serious side effects, although the area where the needle enters the skin may feel a little sore afterwards.
Sacral nerve stimulation (SNS)
This is sometimes called Sacral Neuromodulation (SNM). A small wire (called an electrode) is surgically placed against the sacral nerve in your lower back. The other end of the wire is connected to a small box (called a stimulation box). The SNS device makes mild electrical pulses that stimulate the sacral nerve to help you regain control of your bladder.
This treatment may help to reduce how often you urinate and leak urine. It is quite a new treatment and is only offered at some hospitals.
You will need two operations to fit the SNS device. Both are usually done under local anaesthetic or sedation. In your first operation, the electrode will be connected to a temporary stimulator box placed outside the body. This is to see if SNS works for you. You will have this device for two to four weeks. Depending on whether the SNS device worked for you, the second operation will either be to put in a permanent device, or remove the temporary one.
In the second operation, they will reopen the cut made in your lower back to put in a stimulator box about the size of a two-pound coin under the skin. This is connected to the electrode touching the sacral nerve.
Like all treatments there are risks in having a SNS device, such as infection, pain or discomfort where the SNS device has been put in or parts of the device breaking. SNS is not suitable for everyone. Your doctor will talk to you about whether you’re suitable for SNS.
Botulinum toxin (BOTOX®)
Injecting BOTOX® into the wall of the bladder can help stop the bladder squeezing out urine before it’s full. This is quite a new treatment for urinary frequency and urgency and it’s not available in all hospitals.
Difficulty urinating
Some men find it hard to empty their bladder properly after radiotherapy – this is called urine retention. This may be more likely if you have an enlarged prostate. Radiotherapy, particularly brachytherapy, can cause the prostate to swell and block the urethra, leading to urine retention. It can also cause the urethra to become narrow – this is called a stricture.
A small number of men may get urine retention after radical prostatectomy, HIFU and cryotherapy.
Chronic urine retention
This is where you can’t empty your bladder fully, but can still urinate a little. The first signs often include:
- leaking urine at night
- feeling that your abdomen (stomach area) is swollen
- feeling that you’re not emptying your bladder fully
- a weak flow when you urinate.
Tell your doctor or nurse if you get any of these symptoms. Chronic urine retention is usually painless, but the pressure of the urine can cause the bladder muscles to slowly stretch and become weaker. This can cause urine to be left behind in the bladder when you urinate. You may be more likely to get urine infections, bladder stones, blood in your urine or kidney problems.
Treatments for chronic urine retention include:
- a catheter to drain urine from the bladder
- drugs (alpha blockers or 5-alpha-reductase inhibitors)
- drugs called 5-alpha-reductase inhibitors, which shrink the prostate
- surgery to widen the urethra or the opening of the bladder.
Acute urine retention
This is when you suddenly and painfully can’t urinate – it needs treating straight away. If this happens, call your doctor or nurse, or go to your nearest accident and emergency (A&E) department. They may need to drain your bladder using a catheter.. Make sure they know what prostate cancer treatment you’ve had, especially if you have recently had a radical prostatectomy.
Problems after high intensity focused ultrasound (HIFU)
You’re more likely to get urinary problems after HIFU if you’ve already had other treatments for prostate cancer. Possible urinary problems include:
- difficulty urinating
- leaking urine
- urine infections.
Difficulty urinating
HIFU usually causes the prostate to swell for a week or two, so you’ll have a catheter to drain urine from your bladder until the swelling has gone. HIFU can also cause the urethra to become narrow, making it difficult to empty your bladder (urine retention).
Leaking urine
HIFU can cause some men to leak urine when they cough, sneeze or exercise (stress incontinence). This may be more likely if you’ve already had radiotherapy. There are ways to manage leaking urine.
Urine infections
Some men get a urine infection after HIFU. If this happens, you’ll be given a course of antibiotics to clear the infection.
Problems after cryotherapy
You’re more likely to get urinary problems after cryotherapy if you’ve already had radiotherapy. Possible urinary problems include:
- difficulty urinating
- leaking urine.
Difficulty urinating
Cryotherapy can cause the prostate to swell, making it difficult to urinate for a week or two. You’ll have a catheter to drain urine from your bladder until the swelling has gone. Cryotherapy may also cause the urethra or the opening of the bladder to become narrow. If this happens, you may have a weak or slow flow of urine, or you might not be able to urinate at all. This is known as urine retention.
Leaking urine
A small number of men who have cryotherapy may leak urine. This is more likely if you’ve already had radiotherapy. There are ways to manage leaking urine.
How can I help myself?
Urinary problems can affect your self-esteem and independence, and affect your work, social and sex life.
Making some changes to your lifestyle may help, and there are some practical steps that can make things easier.
- Drink plenty of fluids. Aim to drink about 1.5 to 2 litres (3 to 4 pints) a day. You may worry about drinking lots if you’re leaking urine, but it can help prevent bladder irritation and infection. If your urine is dark, this could be a sign that you need to drink more.
- Cut down on fizzy drinks, alcohol and drinks that contain caffeine (tea, coffee and cola), as these can irritate the bladder.
- Regular pelvic floor muscle exercises can help strengthen the muscles that control when you urinate, and help if you leak urine. Read more in our fact sheet, Pelvic floor muscle exercises.
- Try to maintain a healthy weight. Being overweight can put pressure on your bladder and pelvic floor muscles. You may find our fact sheet, Diet and physical activity for men with prostate cancer, helpful.
- Eat foods that are high in fibre and drink plenty of fluids to avoid constipation (difficulty emptying your bowels), as this can put pressure on your pelvic floor muscles.
- If you smoke try to stop as this can cause coughing, which puts pressure on your pelvic floor muscles. The NHS website has more information about stopping smoking.
- If you often need to use the toilet at night, leave a light on in case you’re in a hurry, or keep a container near your bed.
- Plan ahead when you go out. For example, find out where there are public toilets before leaving home.
- Pack a bag with extra pads, underwear and wet wipes. Some men find it useful to carry a screw-top container in case they can’t find a toilet.
- Get our Urgent toilet card to show to staff in shops, restaurants and other public places. They should let you use their toilets without asking questions. You can order a card on our shop or by calling our Specialist Nurses on 0800 074 8383.
- Disability Rights UK runs a National Key Scheme for anyone with a disability or health condition who needs access to locked public toilets across the UK.
Your GP, specialist nurse or continence nurse can offer you practical and emotional support. You can also speak to our Specialist Nurses. It can sometimes help to talk to other men living with prostate cancer. We have a range of services that can help put you in touch with someone who’s been there and understands what you’re going through. Visit our Who can help page to find out more.
Questions to ask your doctor or nurse
- Is the treatment I’m having for prostate cancer likely to cause any urinary problems?
- What type of urinary problems might I get?
- What should I do if I can’t urinate?
- Will my urinary problems get better?
- What treatments are available?
- What are the risks and side effects of treatments for urinary problems?
- What can I do to help myself?
- Where can I get pads and other products?
Dealing with prostate cancer
Being diagnosed and living with prostate cancer can change how you feel about life. If you or your loved one is dealing with prostate cancer you may feel scared, stressed or even angry. There is no ‘right’ way to feel and everyone reacts differently.
Visit our wellbeing hub for information to help support you in looking after your emotional, mental, and physical wellbeing. If you are close to someone with prostate cancer, find out more about how you can support someone with prostate cancer and where to get more information.
References and reviewers
Updated: March 2022 | Due for Review: March 2025
- Lardas M, Liew M, van den Bergh RC, De Santis M, Bellmunt J, Van den Broeck T, et al. Quality of Life Outcomes after Primary Treatment for Clinically Localised Prostate Cancer: A Systematic Review. Eur Urol. 2017 Dec;72(6):869–85.
- Mottet N, Cornford P, Van den Bergh RCN, Briers E, De Santis M, Fanti S, et al. EAU Guidelines on Prostate Cancer [Internet]. 2020. Available from: https://uroweb.org/guideline/prostate-cancer/
- Ávila M, Patel L, López S, Cortés-Sanabria L, Garin O, Pont À, et al. Patient-reported outcomes after treatment for clinically localized prostate cancer: A systematic review and meta-analysis. Cancer Treat Rev. 2018 May 1;66:23–44.
- Parsons BA, Evans S, Wright MP. Prostate cancer and urinary incontinence. Maturitas. 2009;63(4):323–8.
- Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CMA. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev. 2015;1:CD001843.
- Parihar JS, Ha Y-S, Kim IY. Bladder neck contracture-incidence and management following contemporary robot assisted radical prostatectomy technique. Prostate Int. 2014 Mar;2(1):12–8.
- Wilt TJ, MacDonald R, Rutks I, Shamliyan TA, Taylor BC, Kane RL. Systematic review: comparative effectiveness and harms of treatments for clinically localized prostate cancer. Ann Intern Med. 2008;148(6):435–48.
- Elliott SP, Meng MV, Elkin EP, McAninch JW, Duchane J, Carroll PR. Incidence of Urethral Stricture After Primary Treatment for Prostate Cancer: Data From CaPSURE. J Urol. 2007 Aug;178(2):529–34.
- Simhan J, Ramirez D, Hudak SJ, Morey AF. Bladder neck contracture. Transl Androl Urol. 2014;3(2):214.
- Breyer BN, Davis CB, Cowan JE, Kane CJ, Carroll PR. Incidence of bladder neck contracture after robot-assisted laparoscopic and open radical prostatectomy. BJU Int. 2010;106(11):1734–8.
- Reynard J, Brewster S, Biers S. Oxford Handbook of Urology. 3rd ed. Oxford University Press; 2013.
- Solomon CG, Schaeffer AJ, Nicolle LE. Urinary Tract Infections in Older Men. N Engl J Med. 2016 Feb 11;374(6):562–71.
- Bonkat G, Bartoletti R, Bruyère F, Cai T, Geerlings SE, Koves B, et al. EAU Guidelines on Urological infections [Internet]. European Association of Urology; 2020 [cited 2020 Dec 1]. Available from: https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Urological-infections-2020.pdf
- Kidd EA, Stewart F, Kassis NC, Hom E, Omar MI. Urethral (indwelling or intermittent) or suprapubic routes for short-term catheterisation in hospitalised adults. In: The Cochrane
- Collaboration, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2015 [cited 2016 May 26]. Available from: http://doi.wiley.com/10.1002/14651858.CD004203.pub3
- Tenke P, Mezei T, Bőde I, Köves B. Catheter-associated Urinary Tract Infections. Eur Urol Suppl. 2017 Apr;16(4):138–43.
- Bauer RM, Gozzi C, Hübner W, Nitti VW, Novara G, Peterson A, et al. Contemporary Management of Postprostatectomy Incontinence. Eur Urol. 2011 Jun;59(6):985–96.
- Thiruchelvam N, Cruz F, Kirby M, Tubaro A, Chapple CR, Sievert K-D. A review of detrusor overactivity and the overactive bladder after radical prostate cancer treatment. BJU Int. 2015 Dec;116(6):853–61.
- Macaulay M, Broadbridge J, Gage H, Williams P, Birch B, Moore KN, et al. A trial of devices for urinary incontinence after treatment for prostate cancer. BJU Int. 2015 Sep;116(3):432–42.
- Arroyo Fernández R, García-Hermoso A, Solera-Martínez M, Martín Correa MT, Ferri Morales A, Martínez-Vizcaíno V. Improvement of Continence Rate with Pelvic Floor Muscle Training Post-Prostatectomy: A Meta-Analysis of Randomized Controlled Trials. Urol Int. 2014 Nov 22;94(2):125–32.
- Nazarko L. Male urinary incontinence management: penile sheaths. 2018;23(3):5.
- National Institute for Health and Care Excellence. Lower urinary tract symptoms in men: management. 2010.
- Welk BK, Herschorn S. The male sling for post-prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int. 2012;109(3):328–44.
- Van Bruwaene S, De Ridder D, Van der Aa F. The use of sling vs sphincter in post-prostatectomy urinary incontinence: Sling vs AUS in PPUI. BJU Int. 2015 Sep;116(3):330–42.
- Dosanjh A, Baldwin S, Mytton J, King D, Trudgill N, Belal M, et al. A national study of artificial urinary sphincter and male sling implantation after radical prostatectomy in England. BJU Int. 2020;125(3):467–75.
- American Medical Systems. AdVance XP Male Sling System: instructions for use. American Medical Systems, Inc.; 2012.
- Chung ASJ, Suarez OA, McCammon KA. AdVance male sling. Transl Androl Urol. 2017 Aug;6(4):674–81.
- Romano SV, Metrebian SE, Vaz F, Muller V, D’Ancona CA, Costa De Souza EA, et al. An adjustable male sling for treating urinary incontinence after prostatectomy: a phase III multicentre trial. BJU Int. 2006;97(3):533–9.
- Crivellaro S, Morlacco A, Bodo G, Agro’ EF, Gozzi C, Pistolesi D, et al. Systematic review of surgical treatment of post radical prostatectomy stress urinary incontinence: Systematic review of male SUI surgical treatment. Neurourol Urodyn. 2015 Sep;n/a-n/a.
- Silva LA, Andriolo RB, Atallah ÁN, da Silva EM. Surgery for stress urinary incontinence due to presumed sphincter deficiency after prostate surgery. Cochrane Database Syst Rev. 2014;(9).
- Abrams P, Shearer K. The MASTER trial: artificial urinary sphincter versus male sling. Trends Urol Mens Health. 2015;6(2):37–8.
- Radadia KD, Farber NJ, Shinder B, Polotti CF, Milas LJ, Tunuguntla H. Management of Postradical Prostatectomy Urinary Incontinence: A Review. Urology. 2017;
- Boswell TC, Elliott DS, Rangel LJ, Linder BJ. Long-term device survival and quality of life outcomes following artificial urinary sphincter placement. Transl Androl Urol. 2020 Feb;9(1):56–61.
- Larson T, Jhaveri H, Yeung LL. Adjustable continence therapy (ProACT) for the treatment of male stress urinary incontinence: A systematic review and meta-analysis. Neurourol Urodyn. 2019;38(8):2051–9.
- Kretschmer A, Hübner W, Sandhu JS, Bauer RM. Evaluation and Management of Postprostatectomy Incontinence: A Systematic Review of Current Literature. Eur Urol Focus [Internet]. 2016 Jan [cited 2016 Jul 20]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S2405456916000031
- Burkhard F, Bosch J, Cruz F, Lemack G, Nambiar A, Thiruchelvam N, et al. EAU Guidelines on Urinary Incontinence in Adults. European Association of Urology; 2020.
- Yahya N, Ebert MA, Bulsara M, Haworth A, Kennedy A, Joseph DJ, et al. Dosimetry, clinical factors and medication intake influencing urinary symptoms after prostate radiotherapy: An analysis of data from the RADAR prostate radiotherapy trial. Radiother Oncol. 2015 Jul;116(1):112–8.
- Ishiyama H, Hirayama T, Jhaveri P, Satoh T, Paulino AC, Xu B, et al. Is There an Increase in Genitourinary Toxicity in Patients Treated With Transurethral Resection of the Prostate and Radiotherapy?: A Systematic Review. Am J Clin Oncol. 2014 Jun;37(3):297–304.
- Villeirs L, Tailly T, Ost P, Waterloos M, Decaestecker K, Fonteyne V, et al. Hyperbaric oxygen therapy for radiation cystitis after pelvic radiotherapy: Systematic review of the recent literature. Int J Urol. 2020;27(2):98–107.
- Kolla SB, Dash A. Radiation Cystitis: Acute and Chronic. In: Ehrenpreis ED, Marsh R de W, Small W, editors. Radiation Therapy for Pelvic Malignancy and its Consequences [Internet]. New York, NY: Springer New York; 2015 [cited 2016 Jun 10]. p. 111–8. Available from: http://link.springer.com/10.1007/978-1-4939-2217-8_7
- Thompson A, Adamson A, Bahl A, Borwell J, Dodds D, Heath C, et al. Guidelines for the diagnosis, prevention and management of chemical- and radiation-induced cystitis. J Clin Urol. 2014;7(1):25–35.
- Zerbib M, Zelefsky MJ, Higano CS, Carroll PR. Conventional Treatments of Localized Prostate Cancer. Urology. 2008;72(6):S25–35.
- Jarosek SL, Virnig BA, Chu H, Elliott SP. Propensity-weighted Long-term Risk of Urinary Adverse Events After Prostate Cancer Surgery, Radiation, or Both. Eur Urol. 2015 Feb;67(2):273–80.
- Pascoe C, Duncan C, Lamb BW, Davis NF, Lynch TH, Murphy DG, et al. Current management of radiation cystitis: a review and practical guide to clinical management. BJU Int. 2019;123(4):585–94.
- Smit S, Heyns C. Management of radiation cystitis. Nat Rev Urol. 2010;7:206–14.
- Ohri N, Dicker AP, Showalter TN. Late toxicity rates following definitive radiotherapy for prostate cancer. Can J Urol. 2012;19(4):6373.
- Newman DK, Guzzo T, Lee D, Jayadevappa R. An evidence-based strategy for the conservative management of the male patient with incontinence: Curr Opin Urol. 2014 Nov;24(6):553–9.
- Newman DK, Burgio KL, Markland AD, Goode PS. Urinary Incontinence: Nonsurgical Treatments. In: Griebling TL, editor. Geriatric Urology [Internet]. New York, NY: Springer New York; 2014 [cited 2016 Jun 13]. p. 141–68. Available from: http://link.springer.com/10.1007/978-1-4614-9047-0_11
- Bradley CS, Erickson BA, Messersmith EE, Pelletier-Cameron A, Lai HH, Kreder KJ, et al. Evidence of the Impact of Diet, Fluid Intake, Caffeine, Alcohol and Tobacco on Lower Urinary Tract Symptoms: A Systematic Review. J Urol. 2017 Nov;198(5):1010–20.
- Payne H, Adamson A, Bahl A, Borwell J, Dodds D, Heath C, et al. Chemical- and radiation-induced haemorrhagic cystitis: current treatments and challenges. BJU Int. 2013;
- Hamilton K, Bennett NC, Purdie G, Herst PM. Standardized cranberry capsules for radiation cystitis in prostate cancer patients in New Zealand: a randomized double blinded, placebo controlled pilot study. Support Care Cancer. 2015 Jan;23(1):95–102.
- Gacci M, Saleh O, Giannessi C, Chini T, Della Camera PA, Detti B, et al. Bladder Instillation Therapy With Hyaluronic Acid and Chondroitin Sulfate Improves Symptoms of Postradiation Cystitis: Prospective Pilot Study. Clin Genitourin Cancer. 2016 Feb 8;
- Budäus L, Bolla M, Bossi A, Cozzarini C, Crook J, Widmark A, et al. Functional outcomes and complications following radiation therapy for prostate cancer: a critical analysis of the literature. Eur Urol. 2012;61(1):112–27.
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults (Review). Cochrane Database Syst Rev. 2004;(1).
- Rai BP, Cody JD, Alhasso A, Stewart L. Anticholinergic drugs versus non-drug active therapies for non-neurogenic overactive bladder syndrome in adults (Review). Cochrane Database Syst Rev. 2012;(12).
- Drake MJ, Nitti VW, Ginsberg DA, Brucker BM, Hepp Z, McCool R, et al. Comparative assessment of the efficacy of onabotulinumtoxinA and oral therapies (anticholinergics and mirabegron) for overactive bladder: a systematic review and network meta-analysis. BJU Int. 2017;120(5):611–22.
- National Institute for Health and Care Excellence. Mirabegron for treating symptoms of overactive bladder: Technical appraisal [Internet]. 2013. Available from: https://www.nice.org.uk/Guidance/ta290
- Chen H-L, Chen T-C, Chang H-M, Juan Y-S, Huang W-H, Pan H-F, et al. Mirabegron is alternative to antimuscarinic agents for overactive bladder without higher risk in hypertension: a systematic review and meta-analysis. World J Urol. 2018 Aug 1;36(8):1285–97.
- Gaziev G, Topazio L, Iacovelli V, Asimakopoulos A, Di Santo A, De Nunzio C, et al. Percutaneous tibial nerve stimulation (PTNS) efficacy in the treatment of lower urinary tract dysfunctions: a systematic review. BMC Urol. 2013;13(1):1.
- Stewart F, Gameiro OL, El Dib R, Gameiro MO, Kapoor A, Amaro JL. Electrical stimulation with non-implanted electrodes for overactive bladder in adults. The Cochrane Collaboration, editor. Cochrane Database Syst Rev [Internet]. 2016 Apr 2 [cited 2016 Jul 28]; Available from: http://doi.wiley.com/10.1002/14651858.CD010098.pub3
- Moossdorff-Steinhauser HFA, Berghmans B. Effects of percutaneous tibial nerve stimulation on adult patients with overactive bladder syndrome: a systematic review. Neurourol Urodyn. 2013;32(3):206–14.
- National Institute for Health and Care Excellence. Percutaneous posterior tibial nerve stimulation for overactive bladder syndrome. Interventional procedure guidance 362. 2010.
- Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst Rev. 2011;
- Habashy D, Losco G, Tse V, Collins R, Chan L. Botulinum toxin (OnabotulinumtoxinA) in the male non-neurogenic overactive bladder: clinical and quality of life outcomes. BJU Int. 2015 Oct;116:61–5.
- Moore D, Cohn J, Dmochowski R. Use of Botulinum Toxin A in the Treatment of Lower Urinary Tract Disorders: A Review of the Literature. Toxins. 2016 Mar 23;8(4):88.
- Rancati T, Palorini F, Cozzarini C, Fiorino C, Valdagni R. Understanding Urinary Toxicity after Radiotherapy for Prostate Cancer: First Steps Forward. Tumori J. 2017 Sep;103(5):395–404.
- Lukka H, Waldron T, Chin J, Mayhew L, Warde P, Winquist E, et al. High-intensity Focused Ultrasound for Prostate Cancer: a Systematic Review. Clin Oncol. 2011 Mar;23(2):117–27.
- Negro CL, Muir GH. Chronic urinary retention in men: how we define it, and how does it affect treatment outcome. BJU Int. 2012;110(11):1590–4.
- Gravas S, Cornu JN, Gacci M, Gratzke C, Herrmann TRW, Mamoulakis C, et al. EAU Guidelines on Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO) [Internet]. European Association of Urology; 2020 [cited 2020 Nov 26]. Available from: https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Non-Neurogenic-Male-LUTS-incl.-BPO-2020.pdf
- Jassim Y, Almallah Z. Incomplete emptying of the bladder and retention of urine. Trends Urol Gynaecol Sex Health. 2009;14(3):20–2.
- Gravas S, Bach T, Bachmann A, Drake M, Gacci M, Gratzke C, et al. Guidelines on non-neurogenic male lower urinary tract symptoms (LUTS) including benign prostatic obstruction [Internet]. European Association of Urology; 2016. Available from: https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/
- Yoon PD, Chalasani V, Woo HH. Systematic review and meta-analysis on management of acute urinary retention. Prostate Cancer Prostatic Dis. 2015 Dec;18(4):297–302.
- Morton G, Chung HT, McGuffin M, Helou J, D’Alimonte L, Ravi A, et al. Prostate high dose-rate brachytherapy as monotherapy for low and intermediate risk prostate cancer: Early toxicity and quality-of life results from a randomized phase II clinical trial of one fraction of 19 Gy or two fractions of 13.5 Gy. Radiother Oncol. 2017 Jan 1;122(1):87–92.
- British Uro-oncology Group (BUG), British Association of Urological Surgeons (BAUS). Multi-disciplinary Team (MDT) Guidance for Managing Prostate Cancer. 2013.
- He Y, Tan P, He M, Hu L, Ai J, Yang L, et al. The primary treatment of prostate cancer with high-intensity focused ultrasound. Medicine (Baltimore) [Internet]. 2020 Oct 9 [cited 2020 Nov 25];99(41). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7544371/
- Crouzet S, Blana A, Murat FJ, Pasticier G, Brown SCW, Conti GN, et al. Salvage high-intensity focused ultrasound (HIFU) for locally recurrent prostate cancer after failed radiation therapy: Multi-institutional analysis of 418 patients. BJU Int. 2017;119(6):896–904.
- Uchida T, Nakano M, Hongo S, Shoji S, Nagata Y, Satoh T, et al. High-intensity focused ultrasound therapy for prostate cancer: HIFU and prostate cancer. Int J Urol. 2012 Mar;19(3):187–201.
- Alongi F, De Bari B, Campostrini F, Arcangeli S, Matei DV, Lopci E, et al. Salvage therapy of intraprostatic failure after radical external-beam radiotherapy for prostate cancer: A review. Crit Rev Oncol Hematol. 2013 Dec;88(3):550–63.
- Yutkin V, Ahmed HU, Donaldson I, McCartan N, Siddiqui K, Emberton M, et al. Salvage High-intensity Focused Ultrasound for Patients With Recurrent Prostate Cancer After Brachytherapy. Urology. 2014 Nov;84(5):1157–62.
- Ziglioli F, Baciarello M, Maspero G, Bellini V, Bocchialini T, Cavalieri D, et al. Oncologic outcome, side effects and comorbidity of high-intensity focused ultrasound (HIFU) for localized prostate cancer. A review. Ann Med Surg. 2020 Aug 1;56:110–5.
- Jung JH, Risk MC, Goldfarb R, Reddy B, Coles B, Dahm P. Primary cryotherapy for localised or locally advanced prostate cancer. Cochrane Database Syst Rev [Internet]. 2018 [cited 2018 Sep 6];(5). Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005010.pub3/abstract
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management. NICE guideline 131. 2019.
- de Castro Abreu AL, Bahn D, Leslie S, Shoji S, Silverman P, Desai MM, et al. Salvage focal and salvage total cryoablation for locally recurrent prostate cancer after primary radiation therapy. BJU Int. 2013 Aug;112(3):298–307.
- Levy D, Avallone A, Jones JS. Current state of urological cryosurgery: prostate and kidney. BJU Int. 2010;105(5):590–600.
- Mundy AR, Andrich DE. Posterior urethral complications of the treatment of prostate cancer. BJU Int. 2012;110(3):304–25.
- Caso JR, Tsivian M, Mouraviev V, Kimura M, Polascik TJ. Complications and postoperative events after cryosurgery for prostate cancer. BJU Int. 2012;109(6):840–5.
- National Institute for Health and Clinical Excellence. Cryotherapy for recurrent prostate cancer. Interventional procedure guidance 119. 2005.
- Aus G, Pileblad E, Hugosson J. Cryosurgical ablation of the prostate: 5-year follow-up of a prospective study. Eur Urol. 2002;42(2):133–8.
- Shelley M, Wilt T, Coles B, Mason M. Cryotherapy for localised prostate cancer (Review). The Cochrane Collaboration, editor. Cochrane Database Syst Rev. 2007;(3).
- Glover L, Gannon K, McLoughlin J, Emberton M. Men’s experiences of having lower urinary tract symptoms: factors relating to bother. BJU Int. 2004;94(4):563–7.
- Spendelow JS, Eli Joubert H, Lee H, Fairhurst BR. Coping and adjustment in men with prostate cancer: a systematic review of qualitative studies. J Cancer Surviv. 2018;12(2):155–68.
- Vinod Nargund, Consultant Urological Surgeon, The Princess Grace Hospital
- Anna Ashfield, Prostate Cancer Clinical Nurse Specialist, Guys and St Thomas’ NHS Hospital Foundation Trust
- our Specialist Nurses
- our volunteers.

