How hormone therapy affects you
Like all treatments, hormone therapy can cause side effects. Make sure you discuss these with your doctor or nurse before you start treatment. You can also talk to our Specialist Nurses about side effects.
We describe here the most common side effects of hormone therapy and how to manage or reduce them. It may seem like there are a lot of possible side effects, but you may not get all of them. Hormone therapy affects men in different ways. Some men have fewer side effects than others. This doesn’t mean that the treatment is any less effective.
There are treatments and support to help manage side effects. And some men find that their side effects get better or become easier to deal with over time. The risk of getting each side effect depends on your type of hormone therapy and how long you take it for. If you have hormone therapy alongside another treatment, you may get side effects from both treatments.
Watch Bruce's story about how hormone therapy affected him:
Living with hormone therapy booklet
This booklet is for men who are having hormone therapy for prostate cancer, their partners and families.
Why does hormone therapy cause side effects?
If testosterone is taken away or blocked by hormone therapy, prostate cancer cells will usually shrink, wherever they are in the body. But reducing or blocking testosterone can cause other things to change in your body too.
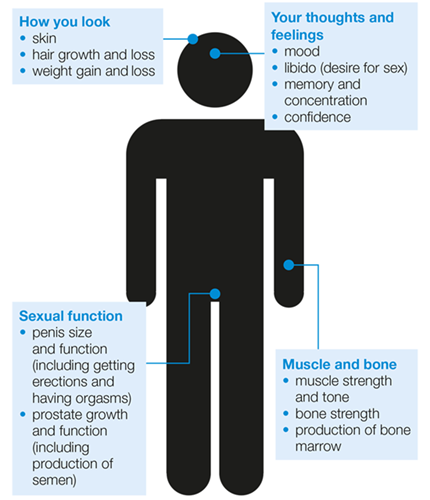
Testosterone controls the development and growth of the sexual organs, including the prostate, and affects the way you think and feel. It also controls other male characteristics, such as erections and muscle strength. So when testosterone is reduced, or taken away by hormone therapy, all of these things can change.
The diagram below shows how testosterone affects a man's body. Knowing this can help you understand what side effects you might get when you're having hormone therapy.
The side effects of hormone therapy are caused by lowered testosterone levels. Side effects will usually last for as long as you are on hormone therapy. If you stop your hormone therapy, your testosterone levels will gradually rise again and some side effects will reduce. Your side effects won’t stop as soon as you finish hormone therapy – it may take several months.
Surgery to remove the testicles (orchidectomy) can’t be reversed, so the side effects are permanent. But there are treatments that can help reduce or manage some of the side effects.
Hot flushes
Hot flushes are a common side effect of hormone therapy and can affect men on LHRH agonists or anti-androgens. Up to eight out of ten men on LHRH agonists (80 per cent) get hot flushes. Some men find that their hot flushes get milder and happen less often over time, but other men continue to have hot flushes for as long as they have hormone therapy.
Hot flushes can vary from a few seconds of feeling overheated to a few hours of sweating, which can be uncomfortable. You might feel very hot in your face, neck, chest or back. They are sometimes described as being mild, moderate or severe.
- A mild hot flush could last for less than three minutes and may make you feel warmer than usual and a little uncomfortable.
- A moderate hot flush can cause you to feel too hot. You might sweat and find you need to take off some layers of clothes.
- A severe hot flush can make you feel very hot and sweaty and you may need to change your clothes or bedding. Some men can feel irritable, uncomfortable, or even sick (nauseous).
Hot flushes might happen suddenly without warning, or they may be triggered by things such as stress, a hot drink or a change in the temperature. You may find you feel cold, shivery or exhausted afterwards. You might also sweat at night, which can disrupt your sleep and cause tiredness.
If your hot flushes are mild or don’t bother you, you may not need treatment. But speak to your doctor or nurse if you find them disruptive or difficult to deal with.
What can help?
There are some lifestyle changes that may help.
- If you smoke, try to stop. Speak to your GP for help stopping or visit the NHS website.
- Try to stay a healthy weight. Read more about diet and physical activity.
- Make sure you drink enough – aim for around six to eight glasses of water a day. Try to cut down on alcohol and drinks that contain caffeine, like tea and coffee.
- Eat less spicy food.
- Keep your room at a cool temperature and use a fan.
- Wear cotton clothes, especially at night.
- Use light cotton bed sheets. If you sweat a lot at night, try using a cotton towel on top of your sheets which you can change easily.
- Try having lukewarm baths and showers rather than hot ones.
You might find it helpful to keep a diary of your symptoms for a few weeks. This can help you work out if there are any situations, or particular drinks or foods that bring on a hot flush. A diary might also help you to decide whether to have treatment for your hot flushes – you can download a diary from our website.
There are medicines that may help relieve the symptoms of hot flushes and reduce how often you get them. Your doctor or nurse may suggest a medicine called medroxyprogesterone or cyproterone acetate. Examples of other medicines that are sometimes used include gabapentin, venlafaxine and paroxetine.
As with any drug, you may get side effects from these medicines. Talk to your doctor or nurse about these before starting any treatment for hot flushes. Some medicines may not be suitable for men who have a history of high blood pressure, heart disease or strokes, or problems with their liver. Your doctor or nurse will discuss this with you.
Complementary therapies are used alongside standard treatments (often called conventional treatments), rather than instead of them. There are many different complementary therapies available that might help with hot flushes. These include acupuncture, hypnotherapy, cognitive behavioural therapy, herbal remedies and homeopathy. But the evidence for most complementary therapies isn’t very strong and we need more research to understand the possible risks and benefits.
It's important to tell your doctor about any complementary therapy you use or are thinking about using. Some complementary therapies have side effects or may interfere with your cancer treatment. You should also tell your complementary therapist about any cancer treatments you are having.
When you choose a therapist, make sure they are properly trained and belong to a professional body. The Complementary and Natural Healthcare Council can give you advice about finding a therapist. Some complementary therapies are available on the NHS. Ask your hospital doctor, nurse or GP about this. Many hospices offer complementary therapies too.
Some men find that acupuncture and hypnotherapy help them deal with hot flushes, although we need more research to show whether these treatments work for all men.
- Acupuncture involves inserting very thin, sterile needles just below the skin. This shouldn’t hurt, but you might get a tingling feeling.
- Hypnotherapy is where a therapist talks to you and helps you go into a trance-like state where you feel very relaxed and calm. They then suggest things that might help.
A small study has found that cognitive behavioural therapy (CBT) can help men on hormone therapy deal with their hot flushes and night sweats. CBT is a therapy that helps you manage problems by helping you to think in a positive way. Read more on the NHS website.
Herbal remedies use plants or plant extracts. Some men like to use herbal remedies, such as sage tea, evening primrose oil and red clover, to help with their hot flushes. But there's no evidence that these work, and it's important to check with your doctor that these are safe for you. For example, there is a small chance that a herbal supplement called black cohosh may cause liver damage. This is rare, but you shouldn't take it if you've ever had liver or kidney disease.
Not all herbal remedies in the UK are licensed, and the quality varies a lot. Be very careful when buying herbal remedies over the internet. Many are made outside the UK and may not be high-quality.
Many companies also make claims that aren’t based on proper research. There may be no real evidence that their products work, and some may even be harmful. Remember that even if a product is 'natural', this doesn't mean it is safe. Some herbal remedies may also affect your PSA level, making the PSA test unreliable.
Macmillan Cancer Support and Cancer Research UK have more information on complementary therapies available, and important safety issues to consider when choosing a therapy. For more information about using herbal remedies safely, visit the MHRA website.
I always carry a flask of iced water to drink. It cools you down for a while. The thing about hot flushes is that they disappear just as quickly as they come.
Extreme tiredness (fatigue)
Hormone therapy for prostate cancer can cause extreme tiredness. For some men this can affect their everyday life. Fatigue can affect your energy levels, your motivation and your emotions. Some men find that tiredness can come on quite suddenly, which means that you need to be careful in certain situations – for example, when you are driving. Talk to your doctor or nurse about how tiredness is affecting you. There are ways to help manage it.
Fatigue can also have other causes such as the cancer itself or other conditions, such as a drop in the number of red blood cells (anaemia) or depression.
What can help?
You might find that your tiredness improves over time. And there are changes you can make to your lifestyle that could help, including:
- being as physically active as you can
- organising your day and prioritising the important tasks, like going to medical appointments
- planning activities for when you know you’ll have more energy – maybe first thing in the morning, or in the afternoon after you’ve had a rest
- dealing with any problems sleeping – try to relax before bed by reading or listening to music. It may also help to avoid drinks with caffeine, such as tea and coffee, as these can keep you awake
- eating a well-balanced diet
- complementary therapies.
Read more about fatigue and ways to manage it.
Our Specialist Nurses are here to support you. They can talk to you about your experience of fatigue and the impact it is having on day-to-day life. They can discuss ways to better manage your tiredness.
There is also more information on ways to manage fatigue in our fact sheet, Fatigue and prostate cancer. Or you could use our interactive online guide.
I found exercise was a good way to manage my fatigue. It motivated me and helped keep my spirits up.
Changes to your sex life
Having hormone therapy affects your sex life in different ways. In most cases, these changes last for as long as you are on hormone therapy. It can take up to a year for sexual function to gradually return to normal after stopping hormone therapy. But some men don’t see an improvement after stopping hormone therapy. And if you’ve had surgery to remove the testicles (orchidectomy), these side effects can’t be reversed.
Not everyone will have all the same side effects, but possible changes to your sex life may include the following.
- Less desire for sex (low libido). Hormone therapy will change your sex drive and may mean that you have less interest in sex. This is because hormone therapy lowers your level of testosterone, which is what gives you your sex drive.
- Erection problems. Hormone therapy can cause problems getting or keeping an erection, known as erectile dysfunction (ED). This is less likely if you’re taking anti-androgen tablets on their own. Your GP or doctor or nurse at the hospital can prescribe treatment.
- Changes to ejaculation and orgasm. You may notice that you produce less semen while you are on hormone therapy. You should still be able to have an orgasm, but it might feel different to before treatment. Some men have less intense orgasms when they are having hormone therapy.
- Changes in penis and testicle size. Hormone therapy can make your penis shorter and change the size of your testicles. If you put on weight because of your hormone therapy, you might also find it harder to see your penis. This could mean that you don’t aim so well when urinating. We don’t yet know if these changes improve if you stop having hormone therapy, but early research suggests that your penis length might recover a little.
Read more about possible changes to your sex life.
What can help?
Men deal with these side effects in different ways. Some men find changes to their sex life more difficult to come to terms with than others.
If you have a partner, talking about sex, your thoughts and feelings can help you both deal with any changes. It isn't always easy to talk about sex and relationships, even for a couple who have been together a long time. But it can bring you closer together and make you feel more confident about facing changes and challenges.
If you’re single or starting to think about dating, you may worry about explaining sexual problems, such as difficulty getting erections or changes to your penis size, to someone you don’t know very well. Fear of rejection or being worried about what other people think about you is normal and everyone has their own worries, whether or not they’ve had cancer.
Remember, having sex isn't just about erections or penetrative sex. Men can have orgasms without an erection or ejaculating and some men get pleasure from pleasuring their partner. There isn't just one way to have sex or experience sexual pleasure – have fun and experiment. There are also other, non-sexual ways of being close. This can be as simple as holding hands or trying new activities together.
Yes we still have sex, but in different ways and with a little bit of medical intervention.
Weight gain
Some men put on weight while they are on hormone therapy, particularly around the waist. You may find that you start to put on weight soon after starting hormone therapy. Some men find this physical change difficult, particularly if they’ve never had any problems with their weight in the past.
What can help?
Physical activity and a healthy diet can help you stay a healthy weight. But it can take a long time to lose any weight that you put on during hormone therapy. If you are finding it difficult to lose weight, ask your doctor to refer you to a dietitian or weight loss programme. Or you could join a local weight loss group – spending time with other people who also want to lose weight can be motivating.
I've made some small changes that are making a difference. I’ve got into a pattern of going out for a walk most mornings and come back feeling lighter about my day. I’m getting some exercise and I’m not quite as tired as I was.
Strength and muscle loss
Testosterone plays an important role in the physical make up of men’s bodies. Compared with women, men usually have more muscle and less body fat. Hormone therapy can cause a decrease in muscle tissue and an increase in body fat. This can change the way your body looks and how physically strong you feel.
Some men also experience muscle aches or joint pain while they’re on hormone therapy. This can happen when you lose muscle. Talk to your doctor or nurse if you have any pain in your muscles or joints. They can talk to you about ways to manage it.
What can help?
Regular gentle resistance exercise, such as lifting light weights or using elastic resistance bands, can help to prevent muscle loss and keep your muscles strong. Speak to your doctor before you start any exercise. They may be able to refer you to a physiotherapist or a local exercise programme. If you can’t move about easily, a physiotherapist can give you some gentle exercises to do at home.
Some areas have walking groups that you could join, which could help you improve your strength and meet new people. Read more about diet and physical activity for men with prostate cancer.
Changes to your memory and concentration
If you’re having hormone therapy you may find it difficult to concentrate or focus on certain tasks. Some men also say they struggle to remember things as well as they did before having hormone therapy. You may hear this called brain fog. But we don’t know for sure whether any changes are caused by the hormone therapy or by something else, because the evidence isn’t very strong. For example, feeling tired, stressed, anxious or depressed can all affect your memory and ability to concentrate. Problems with memory and concentration can also happen naturally as you get older.
Whatever the cause, you may find problems with memory or concentration very frustrating. If you’re having problems with your memory, talk to your doctor or nurse. They will be able to suggest things that may help.
What can help?
You might find some of these tips helpful.
- Try keeping lists or reminder notes.
- Try to concentrate on doing just one thing at a time.
- Avoid things that distract you when you need to concentrate on something.
- Try keeping your mind active – for example, by doing crosswords or other puzzles.
- Make sure you eat a well-balanced diet. Gentle physical activity might also help.
- Make sure you get plenty of rest.
My wife gives me some leeway because she knows I forget things. She just gently reminds me, and then tomorrow she will remind again. And eventually I get around to doing it.
Breast swelling and tenderness
Hormone therapy may cause swelling (gynaecomastia) and tenderness in the chest area. This is caused when levels of oestrogen and testosterone change because of hormone therapy. The amount of swelling can vary from a small amount of swelling to noticeably larger breasts. Tenderness can affect one or both sides of the chest and can range from mild sensitivity to long-lasting pain.
For men taking anti-androgen tablets (such as bicalutamide) on their own, breast swelling and tenderness is the most common side effect. If you take oestrogen tablets, you may also get breast swelling. It’s less common if you are having an LHRH agonist or GnRH antagonist, have had surgery to remove the testicles, or are having more than one type of hormone therapy at the same time (combined hormone therapy). Most men taking a high dose of the anti-androgen bicalutamide for more than six months will get breast swelling.
If you put on weight while you’re on hormone therapy, this can also lead to larger breasts.
What can help?
Breast swelling and tenderness can make men feel uncomfortable or embarrassed about their bodies. If you’ve put on weight while having hormone therapy, a balanced diet and regular exercise may help you lose weight, including from your chest area.
There are also treatments available that can help prevent or reduce breast swelling and tenderness, including the following.
- Radiotherapy. If you are about to start long-term anti-androgens, your doctor may suggest treating the breast area with a single low dose of radiotherapy. This can reduce the risk of breast swelling and tenderness. It has to be done within a month of starting hormone therapy because it won’t work once swelling has already happened. Side effects include the skin becoming red, darker or irritated, but this usually clears up in three to five weeks. You may also lose your chest hair in the area that is treated – this might not grow back.
- Tamoxifen tablets. These can be taken once a week to help prevent or treat breast swelling and tenderness in men taking anti-androgen tablets. They work by stopping the hormone oestrogen from reaching the breast tissue. Tamoxifen may be an option if radiotherapy hasn’t helped to prevent breast swelling. You might not be able to have tamoxifen if you're taking oestrogen tablets, because it may stop the oestrogens from working properly. We don’t know how tamoxifen affects other hormone treatments in the long term. If you have hot flushes, some men find that taking tamoxifen tablets can make these worse.
- Surgery. Surgery may also be used to treat breast swelling by removing painful or swollen areas of the breast. This treatment carries a risk of damage to the nipple and a loss of feeling. It’s usually only offered if other treatments haven't helped to reduce the breast swelling. It’s not available at all hospitals, so talk to your doctor or nurse about whether surgery is an option for you.
Bone thinning
Testosterone helps to keep bones strong. Long-term hormone therapy may cause your bones to gradually lose their bulk. LHRH agonists, GnRH antagonists and surgery to remove the testicles (orchidectomy) can all have this effect. This can happen in the first 12 months of beginning treatment and the amount of bone loss may increase the longer you are on treatment. Anti-androgen and oestrogen tablets are less likely to cause bone thinning.
If bone thinning is severe, it can lead to a condition called osteoporosis. This can increase your risk of broken bones (fractures).
Your doctor may suggest you have a type of X-ray before you start hormone therapy to check if any areas of bone tissue are already weak. You may hear this called a DEXA (dual energy X-ray absorptiometry) scan or a bone density scan. Some men may also need to have regular scans while they are having hormone therapy. You can talk to your doctor about whether you might need a scan.
What can help?
If you already have osteoporosis, have a family history of osteoporosis or have had fractures in the past, talk to your doctor before you start hormone therapy. You should also tell your doctor about any other medicines you are taking, in case they might increase your risk of osteoporosis. The Royal Osteoporosis Society has more information on their website.
There are a number of lifestyle changes that may help to reduce your risk of bone thinning and osteoporosis.
- Eat plenty of calcium and vitamin D. Calcium and vitamin D are important for strong bones. You can get calcium from dairy foods (cheese, milk and yoghurt) and non-dairy foods, such as fish where you eat the bones, tofu and green leafy vegetables. Most of your vitamin D is made inside the body when your skin is exposed to sunlight. But it can be difficult for your body to make enough vitamin D, especially in winter. You can also get it from eating oily fish such as sardines, mackerel and salmon, as well as foods with added vitamin D, such as margarine and some breakfast cereals. You may need to take calcium and vitamin D supplements – speak to your doctor about this.
- Cut down on alcohol. Drinking too much can increase your risk of osteoporosis. Guidelines recommend that men should not regularly drink more than 14 units of alcohol a week.
- Stop smoking. Smoking can increase your risk of osteoporosis. Speak to your GP for help to stop, or visit the NHS website.
- Be as active as you can. We don't yet know whether exercise can help to prevent bone thinning in men who are on hormone therapy. But regular exercise may help to keep you strong and prevent falls that could lead to broken bones. Walking, swimming and gentle resistance exercise, such as lifting light weights or using elastic resistance bands, may be particularly good.
- Keep a healthy weight. Men who are underweight have a higher risk of bone thinning.
Bisphosphonates are drugs that can be used to treat osteoporosis caused by hormone therapy. They can also be used to treat bone weakness caused by cancer that has spread to the bones (advanced prostate cancer).
Denosumab (Xgeva®) is a drug that can help manage bone thinning caused by hormone therapy. It might be an option if bisphosphonates aren’t suitable for you and you live in England, Wales or Scotland. If you live in Northern Ireland, your doctor may be able to apply to your local Health and Social Care (HSC) trust for you to have denosumab if they think it is suitable for you. You might hear this called an individual funding request.
Risk of other health problems
Evidence suggests that having hormone therapy might increase the chance of developing heart disease, stroke and type-2 diabetes. There is also some research that suggests having hormone therapy can increase your risk of getting blood clots and anaemia. But more research is needed to help us understand the links between these conditions.
Research shows that hormone therapy can cause:
- an increase in weight, particularly around the waist
- an increase in cholesterol levels
- changes in insulin.
Talk to your hospital doctor and GP about how often you should have general health checks. You may be weighed and have your blood pressure checked regularly. You may also have blood tests to check for diabetes and to measure your cholesterol levels. Your GP may suggest you have these checks about every six months. Or you can ask for them yourself at your GP surgery.
If you already have heart problems or diabetes, talk to your doctor before you start hormone therapy. They will work with you to manage these conditions.
While the risk of getting these conditions may be worrying, it’s important to remember that hormone therapy helps men to live longer by controlling the cancer.
What can help?
A healthy lifestyle can help reduce your risk of heart disease, stroke and type-2 diabetes. This includes:
- eating a healthy diet
- being physically active
- limiting the amount of salt you eat
- stopping smoking
- cutting down on alcohol.
Loss of body hair
Some men lose their body hair while they are on hormone therapy. This is because testosterone plays a role in hair growth. So when testosterone is reduced, you might lose some of it. It’s less common to lose hair from your head, but if you do, any hair loss caused by hormone therapy treatment usually grows back if you stop hormone therapy. We need more research to show how common this side effect is.
How might hormone therapy make me feel?
Hormone therapy itself can affect your mood. You may find that you feel more emotional than usual or just ‘different’ to how you felt before. Some men find that they cry a lot. You may also get mood swings, such as getting tearful and then angry. Just knowing that these feelings are caused by hormone therapy can help.
Everyone’s different – some men are surprised by the side effects and how upsetting they find them. Others have fewer symptoms or are not as worried by them.
Some of the other side effects of hormone therapy are hard to come to terms with. Physical changes, such as putting on weight, or changes to your sex life, might make you feel very different about yourself. Some men say they feel less masculine because of their diagnosis and treatment.
If you’re starting hormone therapy very soon after being diagnosed with prostate cancer, you might still feel upset, shocked, frightened or angry about having cancer. These feelings are normal, and it's okay to feel this way.
Things in your day-to-day life can change because of the hormone therapy. Your relationships with your partner, family and friends might change. Or you might be too tired to do some of the things you used to do.
Some men experience low moods, anxiety or depression. This could be directly caused by the hormone therapy itself, or because you've been diagnosed with prostate cancer. It could also be due to the impact that treatment is having on you and your family.
If your mood is often very low, you are losing interest in things, or your sleep pattern or appetite has changed a lot, speak to your GP or doctor at the hospital. These can be signs of depression and there are treatments available that could help.
What can help?
Some men find their own way to cope and might not want any outside help. Others try to cope on their own because they don’t want to talk about things or are afraid of worrying loved ones. Go easy on yourself, and give yourself time to deal with your feelings.
Sometimes talking about how you feel can help. You might be able to get support from talking to family or friends. Or talking to your doctor or nurse might help. You could also speak in confidence to our Specialist Nurses.
You might find it helps to talk to someone who’s been through something similar. The volunteers on our one-to-one support service have all been affected by prostate cancer. They are trained to listen and offer support over the phone. We have volunteers who have had hormone therapy and can understand what you’re going through. There are also support groups across the country where you can meet others affected by prostate cancer. Most support groups also welcome partners and family members.
You could also join our online community where you can talk to other people with prostate cancer and their families, or simply read previous conversations.
It’s sometimes difficult to talk to people close to you. Some people find it easier to talk to someone they don’t know. Counsellors are trained to listen and can help you find your own way to deal with things. Many hospitals have counsellors or psychologists who specialise in helping people with cancer – ask your doctor or nurse if this is available. You can also refer yourself for counselling on the NHS, or you could see a private counsellor. Visit the NHS website or contact the British Association for Counselling & Psychotherapy to find out more.
There are several lifestyle changes that might help improve your mood and ease feelings of depression and anxiety. These include:
- learning ways to relax such as yoga, mindfulness, or listening to music
- doing regular physical activity – start slowly and pace yourself, maybe just start off by having a short walk
- carrying on with your usual work, hobbies and social activities that you enjoy, or trying something new – some men say this helps them stay happy and relaxed.
You might also find it helpful to go on a course to learn ways to manage side effects, feelings and relationships. Macmillan Cancer Support, Maggies, Self Management UK, Penny Brohn UK and Look Good Feel Better all run free courses for people living with cancer. Ask your doctor or nurse if there are any courses or education sessions for patients in your local area. Some hospitals have support and information services that may run these types of activities for people with cancer.
If you are feeling depressed or anxious, anti-depressant medicines may help. Let your GP know if you think you’re depressed so that they can help find the right treatment for you. Before you start taking any anti-depressants, make sure you tell your GP, doctor or nurse at the hospital about any other medicines or complementary therapies you’re taking. Anti-depressant medicines can sometimes take a few weeks to start working. Until you start feeling better, you may want to try other things as well, such as counselling or meditation.
You and your partner
If you have a partner, they may feel worried, anxious or upset about your cancer. They might feel isolated and find it difficult to tell you how they are feeling in case they worry you. You can get support together. Or sometimes it can be useful to get separate support as well.
Doctors and nurses are always happy for you to bring your partner along to your appointments, and they might be able to tell you about types of support that would suit you both. Many support groups also welcome partners. The charity Relate provides relationship counselling and other support services for couples.
Read our information for partners and family, or order or download our booklet, When you’re close to someone with prostate cancer: A guide for partners and family.
Hormone therapy can make you feel quite down and tearful. But I’ve learnt to recognise when it’s coming on and ways to deal with it.
What will happen while I'm having hormone therapy?
You will have regular check-ups to monitor how well your treatment is working, including regular PSA tests. The PSA test is a simple blood test and is an effective way of monitoring your cancer. Your doctor or nurse will tell you how often you’ll have check-ups. This will depend on the stage of your prostate cancer and any other treatments you are having.
If you’re having treatment to get rid of your cancer
If your PSA level falls and stays low, this usually suggests your treatment has been successful at getting rid of your cancer. How quickly your PSA level falls, and how low, will depend on the treatment you’ve had and will vary from man to man. Your doctor or nurse will keep an eye on any side effects from your treatment. Let them know if there are any changes while you are on hormone therapy, or if you get any new symptoms. If there is a rise in your PSA level, this may be a sign that your cancer has come back. If this happens, there are further treatments available.
If you’re having treatment to control your cancer
If you have advanced prostate cancer and your PSA level falls, this usually suggests your treatment is working. How quickly your PSA level falls, and how low, will vary from person to person. You’ll generally keep having the hormone therapy, even after your PSA has fallen. This is because the hormone therapy is controlling the cancer and if you stop having it, the cancer might grow more quickly.
As well as regular PSA tests, you’ll have other blood tests to see whether the cancer is affecting other parts of your body, such as your liver, kidneys or bones. You may also have scans to monitor how well your cancer is responding to treatment. Your doctor or nurse will also keep an eye on your side effects or symptoms. Let them know if you notice any changes to your health.
If there is a continuous rise in your PSA level, this may be a sign that your hormone therapy is no longer controlling your cancer so well. There are further treatments available, including other types of hormone therapy or a combination of other treatments.
What if I'm struggling with side effects?
There are treatments and support available to help manage side effects. But some men find that their side effects continue to affect their daily life. If this happens, speak to your doctor or nurse. It might be possible to try a different treatment, or to take a break from hormone therapy.
Prostate Cancer UK hosts a Life on Androgen Deprivation Therapy (ADT) class that supports men with prostate cancer living on hormone therapy. You can sign up here.
Intermittent hormone therapy
If you’re on life-long hormone therapy and having problems with side effects, you might be able to have intermittent hormone therapy. This is where you stop hormone therapy when your PSA level is low and steady, and start it again if your symptoms get worse or your PSA starts to rise. It may help to give you a break from some of the side effects, such as hot flushes and sexual problems, and you may feel better in yourself. But it can take several months for side effects to improve, and some men never notice any improvement.
For some men intermittent hormone therapy can be just as effective at treating prostate cancer as continuous treatment. But it isn’t suitable for everyone. And it isn’t an option if you choose surgery (orchidectomy).
There is a risk that having a break from treatment may mean your cancer might grow. Speak to your doctor or nurse about the advantages and disadvantages of intermittent hormone therapy and whether it might be an option for you.
You will need to have your PSA level checked every three months while you’re having a break from treatment. You can have intermittent hormone therapy for as long as it continues to work. Your doctor or nurse will tell you when you need to start treatment again. This will normally be when your PSA rises to 10 ng/ml, or if your symptoms start to get worse. If you do need to start hormone therapy again, you will usually have the same type as before, for at least three to six months.
What if I decide to stop treatment?
The side effects of hormone therapy can be difficult to deal with, and some men feel that they want to stop their treatment. If you are thinking about stopping hormone therapy, talk to your doctor or nurse. They will explain how this could affect your cancer and discuss any other possible treatments with you.
If you do stop having hormone therapy, the side effects won’t stop straight away. It may take several months for the side effects to improve.
I got to the point of wanting to stop the hormone treatment. But I took a look at the things I wasn’t happy about and made some small changes that are making a difference.
References
Updated: August 2022 | Due for Review: November 2023
- Abrahamsen B, Brask-Lindemann D, Rubin KH, Schwarz P. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. BoneKEy Rep. 2014 Sep 3;3:574.
- Abrahamsson PA. Intermittent androgen deprivation therapy in patients with prostate cancer: Connecting the dots. Asian J Urol. 2017 Oct;4(4):208–22.
- Ahmadi H, Daneshmand S. Androgen deprivation therapy: evidence-based management of side effects. BJU Int. 2013 Apr;111(4):543–8.
- Alibhai SMH, Gogov S, Allibhai Z. Long-term side effects of androgen deprivation therapy in men with non-metastatic prostate cancer: A systematic literature review. Crit Rev Oncol Hematol. 2006 Dec;60(3):201–15.
- Artibani W, Porcaro AB, De Marco V, Cerruto MA, Siracusano S. Management of Biochemical Recurrence after Primary Curative Treatment for Prostate Cancer: A Review. Urol Int. 2018;100(3):251–62.
- Asakawa J, Iguchi T, Tamada S, Yasuda S, Ninomiya N, Kato M, et al. A change from gonadotropin releasing hormone antagonist to gonadotropin releasing hormone agonist therapy does not affect the oncological outcomes in hormone sensitive prostate cancer. Basic Clin Androl [Internet]. 2018 Jul 18 [cited 2019 Jun 17];28. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6050721/
- Azoulay L, Yin H, Benayoun S, Renoux C, Boivin JF, Suissa S. Androgen-Deprivation Therapy and the Risk of Stroke in Patients With Prostate Cancer. Eur Urol. 2011 Dec;60(6):1244–50.
- Baumann FT, Zopf EM, Bloch W. Clinical exercise interventions in prostate cancer patients: a systematic review of randomized controlled trials. Support Care Cancer. 2012;20(2):221–33.
- Beck AM, Robinson JW, Carlson LE. Sexual intimacy in heterosexual couples after prostate cancer treatment: What we know and what we still need to learn. Urol Oncol Semin Orig Investig. 2009 Mar;27(2):137–43.
- Beer TM, Armstrong AJ, Rathkopf D, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in Men with Chemotherapy-naïve Metastatic Castration-resistant Prostate Cancer: Extended Analysis of the Phase 3 PREVAIL Study. Eur Urol. 2017 Feb;71(2):151–4.
- Bekelman JE, Mitra N, Handorf EA, Uzzo RG, Hahn SA, Polsky D, et al. Effectiveness of androgen-deprivation therapy and radiotherapy for older men with locally advanced prostate cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2015 Mar 1;33(7):716–22.
- Bosset PO, Albiges L, Seisen T, de la Motte Rouge T, Phé V, Bitker MO, et al. Current role of diethylstilbestrol in the management of advanced prostate cancer. BJU Int. 2012 Dec;110(11c):E826–9.
- Botrel TEA, Clark O, dos Reis RB, Pompeo ACL, Ferreira U, Sadi MV, et al. Intermittent versus continuous androgen deprivation for locally advanced, recurrent or metastatic prostate cancer: a systematic review and meta-analysis. BMC Urol. 2014;14:9.
- Casey RG, Corcoran NM, Larry Goldenberg S. Quality of life issues in men undergoing androgen deprivation therapy: a review. Asian J Androl. 2012 Mar;14(2):226–31.
- Cella D, Ivanescu C, Holmstrom S, Bui CN, Spalding J, Fizazi K. Impact of enzalutamide on quality of life in men with metastatic castration-resistant prostate cancer after chemotherapy: additional analyses from the AFFIRM randomized clinical trial. Ann Oncol. 2015 Jan;26(1):179–85.
- Chaoul A, Milbury K, Sood AK, Prinsloo S, Cohen L. Mind-Body Practices in Cancer Care. Curr Oncol Rep. 2014 Dec;16(12):417.
- Cormie P, Galvão DA, Spry N, Joseph D, Chee R, Taaffe DR, et al. Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: a randomised controlled trial. BJU Int. 2015;115(2):256–66.
- Crawley D, Garmo H, Rudman S, Stattin P, Häggström C, Zethelius B, et al. Association between duration and type of androgen deprivation therapy and risk of diabetes in men with prostate cancer. Int J Cancer. 2016;139(12):2698–704.
- Crouzet S, Chapelon JY, Rouvière O, Mege-Lechevallier F, Colombel M, Tonoli-Catez H, et al. Whole-gland Ablation of Localized Prostate Cancer with High-intensity Focused Ultrasound: Oncologic Outcomes and Morbidity in 1002 Patients. Eur Urol [Internet]. [cited 2013 May 28]; Available from: http://www.sciencedirect.com/science/article/pii/S0302283813004247
- Di Lorenzo G, Autorino R, Perdonà S, De Placido S. Management of gynaecomastia in patients with prostate cancer: a systematic review. Lancet Oncol. 2005 Dec 1;6(12):972–9.
- Dong Z, Wang H, Xu M, Li Y, Hou M, Wei Y, et al. Intermittent hormone therapy versus continuous hormone therapy for locally advanced prostate cancer: a meta-analysis. Aging Male. 2015 Dec;18(4):233–7.
- Dorff TB, Crawford ED. Management and challenges of corticosteroid therapy in men with metastatic castrate-resistant prostate cancer. Ann Oncol. 2013 Jan 1;24(1):31–8.
- Drewe J, Bucher KA, Zahner C. A systematic review of non-hormonal treatments of vasomotor symptoms in climacteric and cancer patients. SpringerPlus [Internet]. 2015 [cited 2018 Nov 23];4(1). Available from: http://www.springerplus.com/content/4/1/65
- Electronic Medicines Compendium. Bicalutamide 150 mg film-coated tablets. - Patient Information Leaflet [Internet]. 2018 [cited 2019 May 20]. Available from: https://www.medicines.org.uk/emc/product/9687/pil
- Electronic Medicines Compendium. Cyprostat 100mg - Patient Information Leaflet [Internet]. 2017 [cited 2019 May 20]. Available from: https://www.medicines.org.uk/emc/product/6249/pil
- Electronic Medicines Compendium. Flutamide 250 mg Tablets - Patient Information Leaflet [Internet]. 2016 [cited 2019 May 20]. Available from: https://www.medicines.org.uk/emc/product/8428/pil
- Elkins GR, Kendrick C, Koep L. Hypnotic Relaxation Therapy for Treatment of Hot Flashes Following Prostate Cancer Surgery: A Case Study. Int J Clin Exp Hypn. 2014 Jul 3;62(3):251–9.
- Elliott S, Latini DM, Walker LM, Wassersug R, Robinson JW. Androgen Deprivation Therapy for Prostate Cancer: Recommendations to Improve Patient and Partner Quality of Life: Improving Life on ADT. J Sex Med. 2010 Sep;7(9):2996–3010.
- Eziefula CU, Grunfeld EA, Hunter MS. ‘You know I’ve joined your club… I’m the hot flush boy’: a qualitative exploration of hot flushes and night sweats in men undergoing androgen deprivation therapy for prostate cancer. Psychooncology. 2013 Dec;22(12):2823–30.
- Fagerlund A, Cormio L, Palangi L, Lewin R, Santanelli di Pompeo F, Elander A, et al. Gynecomastia in Patients with Prostate Cancer: A Systematic Review. PLoS ONE [Internet]. 2015 Aug 26 [cited 2018 Sep 12];10(8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4550398/
- Fang C, Wu CL, Liu SS, Ge L, Bai JL. Efficacy, safety, and dose comparison of degarelix for the treatment of prostate cancer: A systematic review and meta-analysis. World J Meta-Anal. 2016 Jun 26;4(3):69–76.
- Foley E, Baillie A, Huxter M, Price M, Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: A randomized controlled trial. J Consult Clin Psychol. 2010 Feb;78(1):72–9.
- Fradet Y, Egerdie B, Andersen M, Tammela TLJ, Nachabe M, Armstrong J, et al. Tamoxifen as Prophylaxis for Prevention of Gynaecomastia and Breast Pain Associated with Bicalutamide 150 mg Monotherapy in Patients with Prostate Cancer: A Randomised, Placebo-Controlled, Dose–Response Study. Eur Urol. 2007 Jul 1;52(1):106–15.
- Gagliano-Jucá T, Travison TG, Nguyen PL, Kantoff PW, Taplin ME, Kibel AS, et al. Effects of Androgen Deprivation Therapy on Pain Perception, Quality of Life, and Depression in Men With Prostate Cancer. J Pain Symptom Manage. 2018 Feb 1;55(2):307-317.e1.
- Galletti G, Leach BI, Lam L, Tagawa ST. Mechanisms of resistance to systemic therapy in metastatic castration-resistant prostate cancer. Cancer Treat Rev. 2017 Jun;57:16–27.
- Gardner JR, Livingston PM, Fraser SF. Effects of Exercise on Treatment-Related Adverse Effects for Patients With Prostate Cancer Receiving Androgen-Deprivation Therapy: A Systematic Review. J Clin Oncol. 2014 Feb 1;32(4):335–46.
- Grenader T, Plotkin Y, Gips M, Cherny N, Gabizon A. Diethylstilbestrol for the treatment of patients with castration-resistant prostate cancer: Retrospective analysis of a single institution experience. Oncol Rep. 2014 Jan 1;31(1):428–34.
- Gunlusoy B, Ceylan Y, Koskderelioglu A, Gedizlioglu M, Degirmenci T, Ortan P, et al. Cognitive Effects of Androgen Deprivation Therapy in Men With Advanced Prostate Cancer. Urology. 2017 May 1;103:167–72.
- Guo Z, Huang Y, Gong L, Gan S, Chan FL, Gu C, et al. Association of androgen deprivation therapy with thromboembolic events in patients with prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2018 Jul 9;1.
- Haliloglu A, Baltaci S, Yaman O. Penile length changes in men treated with androgen suppression plus radiation therapy for local or locally advanced prostate cancer. J Urol. 2007 Jan;177(1):128–30.
- Haseen F, Murray LJ, Cardwell CR, O’Sullivan JM, Cantwell MM. The effect of androgen deprivation therapy on body composition in men with prostate cancer: Systematic review and meta-analysis. J Cancer Surviv. 2010 Jun 1;4(2):128–39.
- Hicks BM, Klil-Drori AJ, Yin H, Campeau L, Azoulay L. Androgen Deprivation Therapy and the Risk of Anemia in Men with Prostate Cancer: Epidemiology. 2017 Sep;28(5):712–8.
- Higano CS. Side effects of androgen deprivation therapy: monitoring and minimizing toxicity. Urology. 2003;61(2):32–8.
- Hwang TIS, Lin YC, Lee MCC, Juang GD, Yeh CH, Cheng YH, et al. The Effects of Medical Castration on Testes in Patients With Advanced Prostate Cancer. Urol Sci. 2010 Dec;21(4):169–74.
- Irani J, Salomon L, Oba R, Bouchard P, Mottet N. Efficacy of venlafaxine, medroxyprogesterone acetate, and cyproterone acetate for the treatment of vasomotor hot flushes in men taking gonadotropin-releasing hormone analogues for prostate cancer: a double-blind, randomised trial. Lancet Oncol. 2010 Feb;11(2):147–54.
- Iversen P, Karup C, Van der Meulen E, Tanko LB, Huhtaniemi I. Hot flushes in prostatic cancer patients during androgen-deprivation therapy with monthly dose of degarelix or leuprolide. Prostate Cancer Prostatic Dis. 2011;14(2):184–90.
- Jhan JH, Yeh HC, Chang YH, Guu SJ, Wu WJ, Chou YH, et al. New-onset diabetes after androgen-deprivation therapy for prostate cancer: A nationwide propensity score-matched four-year longitudinal cohort study. J Diabetes Complications. 2018 Jul;32(7):688–92.
- Jones JM, Kohli M, Loprinzi CL. Androgen deprivation therapy-associated vasomotor symptoms. Asian J Androl. 2012 Jan 30;14(2):193–7.
- Kadono Y, Nohara T, Kawaguchi S, Sakamoto J, Makino T, Nakashima K, et al. Changes in penile length after radical prostatectomy: effect of neoadjuvant androgen deprivation therapy. Andrology [Internet]. 2018 Jul 2 [cited 2018 Nov 26]; Available from: http://doi.wiley.com/10.1111/andr.12517
- Karling P, Hammar M, Varenhorst E. Prevalence and duration of hot flushes after surgical or medical castration in men with prostatic carcinoma. J Urol. 1994 Oct;152(4):1170–3.
- Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, et al. Effects of resistance exercise in prostate cancer patients: a meta-analysis. Support Care Cancer. 2017 Jun 10;
- Keogh JWL, MacLeod RD. Body Composition, Physical Fitness, Functional Performance, Quality of Life, and Fatigue Benefits of Exercise for Prostate Cancer Patients: A Systematic Review. J Pain Symptom Manage. 2012 Jan;43(1):96–110.
- Klotz L, Boccon-Gibod L, Shore ND, Andreou C, Persson BE, Cantor P, et al. The efficacy and safety of degarelix: a 12-month, comparative, randomized, open-label, parallel-group phase III study in patients with prostate cancer. BJU Int. 2008 Dec;102(11):1531–8.
- Kumar S, Shelley M, Harrison C, Coles B, Wilt T, Mason M. Neo-adjuvant and adjuvant hormone therapy for localised and locally advanced prostate cancer (review). Cochrane Database Syst Rev. 2006;(4).
- Kunath F, Grobe HR, Rücker G, Motschall E, Antes G, Dahm P, et al. Non-steroidal antiandrogen monotherapy compared with luteinising hormone-releasing hormone agonists or surgical castration monotherapy for advanced prostate cancer (review). Cochrane Database Syst Rev. 2014;(6).
- Langston B, Armes J, Levy A, Tidey E, Ream E. The prevalence and severity of fatigue in men with prostate cancer: a systematic review of the literature. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. 2013 Jun;21(6):1761–71.
- Lee MS, Kim KH, Shin BC, Choi SM, Ernst E. Acupuncture for treating hot flushes in men with prostate cancer: a systematic review. Support Care Cancer. 2009 Feb 18;17(7):763–70.
- Litwin MS, Tan HJ. The Diagnosis and Treatment of Prostate Cancer: A Review. JAMA. 2017 Jun 27;317(24):2532.
- Loriot Y, Miller K, Sternberg CN, Fizazi K, De Bono JS, Chowdhury S, et al. Effect of enzalutamide on health-related quality of life, pain, and skeletal-related events in asymptomatic and minimally symptomatic, chemotherapy-naive patients with metastatic castration-resistant prostate cancer (PREVAIL): results from a randomised, phase 3 trial. Lancet Oncol. 2015;16(5):509–21.
- Louda MA, Valis M, Splichalova J, Pacovský J, Khaled B, Podhola M, et al. Psychosocial implications and the duality of life outcomes for patients with prostate carcinoma after bilateral orchiectomy. [Internet]. undefined. 2012 [cited 2018 Sep 7]. Available from: /paper/Psychosocial-implications-and-the-duality-of-life-Louda-Valis/b8c4e31ac3199a32336e7f61a6687bf49cc29c10
- Macherey S, Monsef I, Jahn F, Jordan K, Yuen KK, Heidenreich A, et al. Bisphosphonates for advanced prostate cancer. Cochrane Database Syst Rev [Internet]. 2017 Dec 26 [cited 2018 Jan 5]; Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006250.pub2/abstract
- Magnan S, Zarychanski R, Pilote L, Bernier L, Shemilt M, Vigneault E, et al. Intermittent vs Continuous Androgen Deprivation Therapy for Prostate Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2015 Sep 17;1–10.
- Marzouk S, Naglie G, Tomlinson G, Duff Canning S, Breunis H, Timilshina N, et al. Impact of Androgen Deprivation Therapy on Self-Reported Cognitive Function in Men with Prostate Cancer. J Urol [Internet]. 2018 Mar 1 [cited 2018 Aug 10]; Available from: http://www.sciencedirect.com/science/article/pii/S0022534718393790
- Mason MD, Parulekar WR, Sydes MR, Brundage M, Kirkbride P, Gospodarowicz M, et al. Final Report of the Intergroup Randomized Study of Combined Androgen-Deprivation Therapy Plus Radiotherapy Versus Androgen-Deprivation Therapy Alone in Locally Advanced Prostate Cancer. J Clin Oncol [Internet]. 2015 Feb 17 [cited 2015 May 8]; Available from: http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2014.57.7510
- Mohile SG, Mustian K, Bylow K, Hall W, Dale W. Management of complications of androgen deprivation therapy in the older man. Crit Rev Oncol Hematol. 2009 Jun;70(3):235–55.
- Mottet N, Cornford P, van der Bergh RCN. EAU Guidelines on Prostate Cancer. European Association of Urology; 2022.
- Mottet N, Prayer-Galetti T, Hammerer P, Kattan MW, Tunn U. Optimizing outcomes and quality of life in the hormonal treatment of prostate cancer. BJU Int. 2006 Jul;98(1):20–7.
- Mottet N, Van den Bergh RCN, Briers E, Bourke L, Cornford P, De Santis M, et al. EAU - ESTRO - ESUR - SIOG Guidelines on Prostate Cancer. European Association of Urology; 2018.
- Murad MH, Johnson, Kermott. Gynecomastia - evaluation and current treatment options. Ther Clin Risk Manag. 2011 Mar;145.
- National Institute for Health and Care Excellence. Abiraterone for treating metastatic hormone-relapsed prostate cancer before chemotherapy is indicated. Technology appraisal guidance 387. 2016.
- National Institute for Health and Care Excellence. Degarelix for treating advanced hormone-dependent prostate cancer. Technology appraisal guidance 404 [Internet]. 2016. Available from: https://www.nice.org.uk/guidance/TA404/chapter/1-Recommendations
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management. 2021.
- National Institute for Health and Care Excellence. Prostate Cancer: diagnosis and treatment. Full guideline 175. 2014.
- National Institute for Health and Clinical Excellence. Osteoporosis: assessing the risk of fragility fracture. Short clinical guideline. Clinical guideline 146 [Internet]. 2012 [cited 2015 Nov 16]. Available from: https://www.nice.org.uk/guidance/cg146/evidence/osteoporosis-fragility-fracture-full-guideline-186818365
- Ndibe C, Wang CG, Sonpavde G. Corticosteroids in the Management of Prostate Cancer: A Critical Review. Curr Treat Options Oncol. 2015;16(2).
- Nead KT, Boldbaatar N, Yang DD, Sinha S, Nguyen PL. Association of Androgen Deprivation Therapy and Thromboembolic Events: a Systematic Review and Meta-Analysis. Urology [Internet]. 2018 Jan [cited 2018 Jan 29]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S0090429518300165
- Nead KT, Sinha S, Nguyen PL. Androgen deprivation therapy for prostate cancer and dementia risk: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2017 Sep;20(3):259–64.
- Nead KT, Sinha S, Yang DD, Nguyen PL. Association of androgen deprivation therapy and depression in the treatment of prostate cancer: A systematic review and meta-analysis. Urol Oncol Semin Orig Investig. 2017 Nov 1;35(11):664.e1-664.e9.
- Nguyen PL, Alibhai SMH, Basaria S, D’Amico AV, Kantoff PW, Keating NL, et al. Adverse Effects of Androgen Deprivation Therapy and Strategies to Mitigate Them. Eur Urol. 2015 May;67(5):825–36.
- Nguyen PL, Je Y, Schutz FAB, Hoffman KE, Hu JC, Parekh A, et al. Association of Androgen Deprivation Therapy With Cardiovascular Death in Patients With Prostate Cancer: A Meta-analysis of Randomized Trials. JAMA. 2011 Dec 7;306(21):2359–66.
- NHS Choices. Alcohol units [Internet]. nhs.uk. 2018 [cited 2018 Sep 10]. Available from: https://www.nhs.uk/live-well/alcohol-support/calculating-alcohol-units/
- Oliffe J. Embodied masculinity and androgen deprivation therapy. Sociol Health Illn. 2006 May;28(4):410–32.
- Owen PJ, Daly RM, Livingston PM, Fraser SF. Lifestyle guidelines for managing adverse effects on bone health and body composition in men treated with androgen deprivation therapy for prostate cancer: an update. Prostate Cancer Prostatic Dis. 2017 Jun;20(2):137–45.
- Park KK, Lee SH, Chung BH. The Effects of Long‐Term Androgen Deprivation Therapy on Penile Length in Patients with Prostate Cancer: A Single‐Center, Prospective, Open‐Label, Observational Study. J Sex Med. 2011 Nov;8(11):3214–
- Poole KES, Compston JE. Osteoporosis and its management. BMJ. 2006 Dec 16;333(7581):1251–6.
- Prostate cancer - Treatment [Internet]. nhs.uk. 2017 [cited 2022 Aug 30]. Available from: https://www.nhs.uk/conditions/prostate-cancer/treatment/
- Prostate Cancer UK and Stonewall. Exploring the needs of gay and bisexual men dealing with prostate cancer. 2013.
- Rhee H, Gunter JH, Heathcote P, Ho K, Stricker P, Corcoran NM, et al. Adverse effects of androgen-deprivation therapy in prostate cancer and their management. BJU Int. 2014;115(S5):3–13.
- Ritch CR, Cookson MS. Advances in the management of castration resistant prostate cancer. BMJ. 2016 Oct 17;i4405.
- Saylor PJ, Smith MR. Metabolic Complications of Androgen Deprivation Therapy for Prostate Cancer. J Urol. 2013 Jan;189(1):S34–44.
- Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012 Sep 27;367(13):1187–97.
- Schmidt-Hansen M, Hoskin P, Kirkbride P, Hasler E, Bromham N. Hormone and Radiotherapy versus Hormone or Radiotherapy Alone for Non-metastatic Prostate Cancer: A Systematic Review with Meta-analyses. Clin Oncol. 2014 Oct;26(10):e21–46.
- Schröder F, Crawford ED, Axcrona K, Payne H, Keane TE. Androgen deprivation therapy: past, present and future. BJU Int. 2012 Jun;109 Suppl 6:1–12.
- Serpa Neto A, Tobias-Machado M, Esteves MAP, Senra MD, Wroclawski ML, Fonseca FLA, et al. Bisphosphonate therapy in patients under androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2012;15(1):36–44.
- Sharifi N, Gulley JL, Dahut WL. An Update on Androgen Deprivation Therapy for Prostate Cancer. Endocr Relat Cancer. 2010 Dec;17(4):R305–15.
- Sharpley CF, Christie DRH, Bitsika V. Do hormone treatments for prostate cancer cause anxiety and depression? Int J Clin Oncol. 2014;19(3):523–30.
- Shelley MD, Kumar S, Wilt T, Staffurth J, Coles B, Mason MD. A systematic review and meta-analysis of randomised trials of neo-adjuvant hormone therapy for localised and locally advanced prostate carcinoma. Cancer Treat Rev. 2009 Feb;35(1):9–17.
- Shore ND, Abrahamsson PA, Anderson J, Crawford ED, Lange P. New considerations for ADT in advanced prostate cancer and the emerging role of GnRH antagonists. Prostate Cancer Prostatic Dis. 2013;16(1):7–15.
- Shore ND. Experience with degarelix in the treatment of prostate cancer. Ther Adv Urol. 2012;1756287212461048.
- Smith MR, Egerdie B, Toriz NH, Feldman R, Tammela TLJ, Saad F, et al. Denosumab in Men Receiving Androgen-Deprivation Therapy for Prostate Cancer. N Engl J Med. 2009 Aug 20;361(8):745–55. Healthcare Improvement Scotland. Denosumab for the prevention of skeletal-related events in adults with bone metastases from solid tumours. NICE (Multiple) Technology Appraisal Guidance No 265 [Internet]. [cited 2015 May 13]. Available from: http://www.healthcareimprovementscotland.org/programmes/nice_guidance_and_scotland/mta_resources/appraisal_265.aspx?iru=FV15K62K54
- Stefanopoulou E, Yousaf O, Grunfeld EA, Hunter MS. A randomised controlled trial of a brief cognitive behavioural intervention for men who have hot flushes following prostate cancer treatment (MANCAN). Psychooncology. 2015 Sep;24(9):1159–66.
- Sun M, Cole AP, Hanna N, Mucci LA, Berry DL, Basaria S, et al. Cognitive Impairment in Men with Prostate Cancer Treated with Androgen Deprivation Therapy: A Systematic Review and Meta-Analysis. J Urol. 2018 Jun 1;199(6):1417–25.
- Tavakoli J, Miar S, Majid Zadehzare M, Akbari H. Evaluation of Effectiveness of Herbal Medication in Cancer Care: A Review Study. Iran J Cancer Prev. 2012;5(3):144–56.
- Teschke R, Schwarzenboeck A, Schmidt-Taenzer W, Wolff A, Hennermann KH. Herb induced liver injury presumably caused by black cohosh: A survey of initially purported cases and herbal quality specifications. 2011;11.
- Thorsen L, Courneya KS, Stevinson C, Fosså SD. A systematic review of physical activity in prostate cancer survivors: outcomes, prevalence, and determinants. Support Care Cancer. 2008 Feb 15;16(9):987–97.
- Todenhöfer T, Stenzl A, Hofbauer LC, Rachner TD. Targeting Bone Metabolism in Patients with Advanced Prostate Cancer: Current Options and Controversies. Int J Endocrinol. 2015;2015:1–9.
- Tombal B. A Holistic Approach to Androgen Deprivation Therapy: Treating the Cancer without Hurting the Patient. Urol Int. 2009;83(4):373–8.
- Treanor CJ, Li J, Donnelly M. Cognitive impairment among prostate cancer patients: An overview of reviews. Eur J Cancer Care (Engl). 2017 Nov 1;26(6):e12642.
- Turo R, Smolski M, Esler R, Kujawa ML, Bromage SJ, Oakley N, et al. Diethylstilboestrol for the treatment of prostate cancer: past, present and future. Scand J Urol. 2014 Feb;48(1):4–14.
- Viani GA, Bernardes da Silva LG, Stefano EJ. Prevention of Gynecomastia and Breast Pain Caused by Androgen Deprivation Therapy in Prostate Cancer: Tamoxifen or Radiotherapy? Int J Radiat Oncol. 2012 Jul 15;83(4):e519–24.
- Visapää H. Switching from an LHRH Antagonist to an LHRH Agonist: A Case Report of 10 Finnish Patients with Advanced Prostate Cancer. Oncol Ther. 2017;5(1):119–23.
- Wibowo E, Pollock PA, Hollis N, Wassersug RJ. Tamoxifen in men: a review of adverse events. Andrology. 2016;4(5):776–88.
- Wilkins A, Shahidi M, Parker C, Gunapala R, Thomas K, Huddart R, et al. Diethylstilbestrol in castration-resistant prostate cancer. BJU Int. 2012 Dec 1;110(11b):E727–35.
- Wu LM, Tanenbaum ML, Dijkers MPJM, Amidi A, Hall SJ, Penedo FJ, et al. Cognitive and neurobehavioral symptoms in patients with non-metastatic prostate cancer treated with androgen deprivation therapy or observation: A mixed methods study. Soc Sci Med. 2016 May 1;156:80–9.
- Zhang MF, Wen YS, Liu WY, Peng LF, Wu XD, Liu QW. Effectiveness of Mindfulness-based Therapy for Reducing Anxiety and Depression in Patients With Cancer: A Meta-analysis. Medicine (Baltimore). 2015 Nov;94(45):e0897-0890.
This publication was reviewed and updated by:
- Our Specialist Nurses
- Our Health Information team.

