Research
11 Aug 2022New scanning technique reduces unnecessary biopsies by 90% meaning thousands of men could be spared pain and anxiety, thanks to you.
“It’s rare to see such a big improvement on current practice, both in terms of accuracy and driving down harms caused by testing” says our Research Director Matt Hobbs.
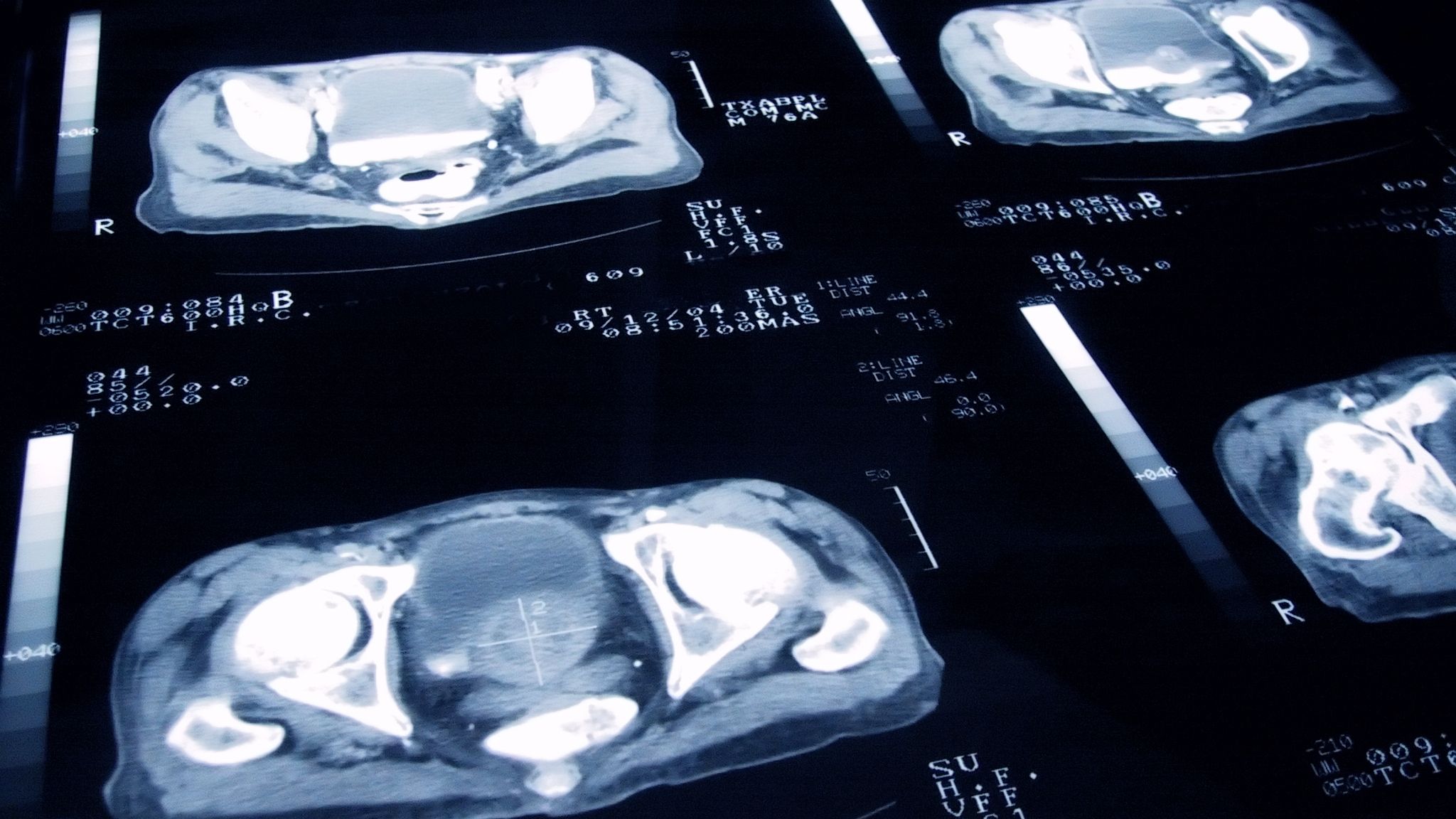
If the results of a PSA blood test suggest that you might have prostate cancer, you will most likely need a prostate biopsy. A biopsy is a procedure in which small samples of the prostate are removed and then looked at with a microscope.
Biopsies are how we diagnose cancer. They allow doctors to take cells to study under a microscope so they can say for certain whether a man has cancer or not. They’re absolutely necessary if we want to save treat cancer and save lives. But they can cause unintended side effects such as infections, as well as causing unnecessary anxiety for men. We want all men who have prostate cancer to have access to a safe, accurate biopsy but we want men who don’t have prostate cancer not to have to have one at all. Many of the men who currently have a biopsy for suspected prostate cancer, turn out not to have cancer at all. That may change soon, thanks to you.
The INNOVATE trial, funded with a £450,000 grant by Prostate Cancer UK and Movember, was based at University College London . Results published last week showed that using an innovative type of scan – called VERDICT MRI – alongside standard imaging techniques was significantly better at identifying men who do not have prostate cancer. These men could safely avoid biopsy altogether, reducing the number of unnecessary biopsies by 90%.
VERDICT (Vascular, Extracellular, and Restricted Diffusion for Cytometry in Tumor) is a new MRI technique that gives additional information about the prostate based on exactly where water molecules are and how they are behaving. This can give a quantitative indication of how “normal” or “abnormal” the cell structure within the prostate is. Aggressive prostate cancer is more likely to result in very abnormal cell structures, so researchers have been able to define a threshold that is likely to be reached only when aggressive prostate cancer is present.

This new technique requires no new equipment – it can be done on MRI scanners already in use and should eventually be possible on all standard 3T scanners, so would be relatively easy to roll out into clinical practice across the UK.
Professor Shonit Punwani is the lead investigator of the INNOVATE trial. Speaking after the results were published last week, he said: “It potentially has the added benefit of reducing the cost of diagnosing prostate cancer to the NHS, which is hugely important given the additional strain on the system caused by the pandemic. Our next step is to use VERDICT MRI in an even bigger study across multiple hospital sites. If successful, the trial should provide the evidence needed to change practice in the NHS in the near future.”
John Aves, 81, from Wrexham, Wales, underwent two biopsies before being diagnosed with prostate cancer in 2014.
John said: “I had been getting up several times in the night to go the toilet for quite a while. I wasn't particularly concerned about my symptoms – I just put it down to 'old man's bladder'. But when I went to my GP for a UTI, he wanted to do some tests for prostate cancer.
“I ended up having a transrectal biopsy which came back negative. My urologist was still certain I had prostate cancer, so he referred me for a template biopsy. I’m lucky he did because that led to my diagnosis. Fortunately, it hadn’t spread and I am now cancer-free.
“Having a biopsy is never the most pleasant experience, so research like this that could improve diagnosis and stop men like me having to undergo multiple or unnecessary procedures is hugely welcome.”
The INNOVATE trial was funded as part of a Prostate Cancer UK and Movember scheme designed to take early-stage research and move it a significant step closer to clinical practice. That’s exactly what we’ve achieved here. Before our grant VERDICT had been tested in only 8 men. Now, through this trial it has been performed on over 300 men.
Dr Sarah Hsiao, Director Biomedical Research and Impact at Movember, said: “It’s yet another win for Prostate Cancer UK’s longstanding partnership with Movember, which has seen us fund over 90 grants together since 2012. Today’s exciting results show that we are now seeing those grants make real improvements for men with prostate cancer.”
Dr Matthew Hobbs, Director of Research at Prostate Cancer UK, added: “It’s rare to see such a big improvement on current practice, both in terms of accuracy and driving down harms caused by testing. These results are a massive leap forward for an exciting new test that could spare thousands of men each year unnecessary anxiety and pain.”
These huge leaps in cancer care that can benefit thousands of men are only possible because of the continued support of people like you. A regular gift will help us transform diagnosis, to catch cancer earlier and save thousands of lives. Will you help us transform diagnosis?


