What to expect
You might have questions about what will happen as your cancer progresses and you approach the end of your life. Knowing what to expect can help you and your family be more prepared.
You might also find it helpful to read about the care and support you can receive.
What should I expect as my cancer progresses?
How does prostate cancer spread?
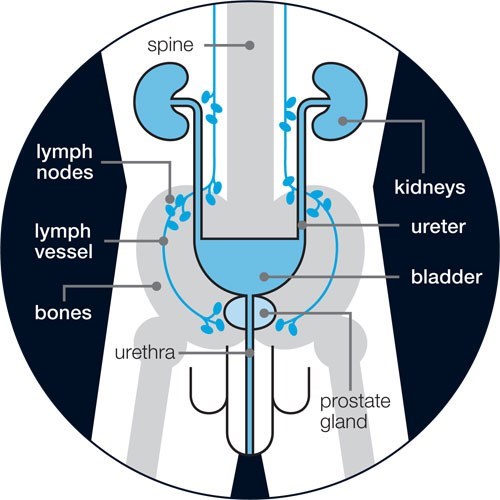
Prostate cancer cells can move from the prostate to other parts of the body through the blood stream. Or they can spread to the lymph nodes near the prostate and then travel through the lymph vessels to other parts of your body. Lymph nodes and lymph vessels are part of your lymphatic system and are found throughout your body.
Prostate cancer most commonly spreads to the bones and lymph nodes. It can also spread to, or press on, the tube you urinate through (urethra), the bladder, the tubes that carry urine from the kidneys to the bladder (ureters) and part of the bowel (rectum). Prostate cancer may spread to other parts of the body, including the lungs and liver. But this is less common.
If tests and scans show that your cancer is spreading, ask your doctor what will happen next. This can help you and your family prepare for what to expect. Find out more about advanced prostate cancer and treatments.
Watch our video about advanced prostate cancer.
How does prostate cancer cause problems?
Prostate cancer can cause problems if it is pressing on your bones or nerves. It can also cause problems by stopping your normal cells from working properly.
What problems can advanced prostate cancer cause?
The symptoms and problems you have will depend on where the cancer has spread to. Even though your cancer is still growing, you will still be able to have treatment to help manage these problems.
Advanced prostate cancer problems may include:
- extreme tiredness (fatigue)
- pain
- urinary problems
- bowel problems
- broken bones (fractures)
- sexual problems
- build up of fluid (lymphoedema)
- low red blood cell levels (anaemia)
- metastatic spinal cord compression (MSCC)
- high calcium levels (hypercalcaemia) – symptoms can include tiredness, feeling and being sick (nausea and vomiting) and difficulty emptying your bowels (constipation)
- eating problems and weight loss.
Some men find that they get more of these problems in their last months and weeks. Others find that existing problems get worse. There are treatments to help manage these problems and things that can help.
What should I look out for?
If you have any pain or notice any changes you’re worried about, speak to your doctor or nurse. You can also read more about problems caused by advanced prostate cancer, or contact our Specialist Nurses.
It's important to be aware of the symptoms of metastatic spinal cord compression (MSCC). This is a very serious medical condition that affects some men with advanced prostate cancer. If you have any symptoms of MSCC, it’s important to get medical advice straight away.
Don’t wait to see if it gets better and don’t worry if it’s an inconvenient time, such as the evening or weekend. If your doctor or nurse isn’t available, go to your nearest accident and emergency (A&E) department. Tell the staff there that you have advanced prostate cancer and that you have MSCC symptoms.
How do I know how long I have left to live?
You might want to know how long you have left to live. This can help you prepare and plan the time you have left. There might be things you want to do or people you want to see. But some men don’t want to know how long they have left. Everyone is different.
You can ask your doctor how long you have left to live. They won’t be able to give you an exact answer. This can be frustrating and it may feel like your doctor is trying to avoid your questions. But no-one can know for certain how long you have left because everyone's body and everyone's cancer is different. However, your doctor will be able to give you some idea based on where the cancer has spread to, how you are responding to treatment, how quickly the cancer has spread, and what problems it is causing.
It can be helpful to talk with your family about this. You may not want to upset them but they might have similar questions and thoughts to you.
If you have months or maybe years left to live, it can be difficult for your doctor to say exactly how long you have left. This is because they don’t know how you will respond to different treatments. If your treatment stops working so well, there may be other treatments available. Some men may not respond well to one treatment, but may respond better to another. Read more about treatments for advanced prostate cancer.
If you have weeks or days left to live, your doctor may have a better idea of how long you might have left. This is because you may have physical changes that suggest you are nearing the end of your life.
If your doctor does give you some idea of how long you have left, it’s important to remember that this is not an exact answer. It can be difficult for you and your family to deal with if you live shorter or longer than they say.
What will happen in the last few days?
It can help to know what is normal in the last few days of life so that you know what to expect. You might not be aware of these changes when they happen because you may be drowsy or unconscious.
If you're supporting someone who is dying, read about what you can do to help and how you can get support.
Pain
Many people worry about being in pain when they are dying. Some people do get pain if their prostate cancer presses on their nerves or makes their bones weak. But not everyone dying from prostate cancer has pain. And if you are in pain, there are things that can help to reduce and manage pain.
You should tell your doctor or nurse if you’re in pain or if your pain gets worse. They can talk with you about how best to manage your pain and can help keep it under control.
You may find sitting or lying in some positions more comfortable than others, so ask if you need help getting into a different position.
Your doctor can give you medicines to help manage pain. The type of medicines they give you will depend on what is causing the pain and which medicines are suitable.
Your doctor will monitor how the pain medicines are working and may change the type of medicine or the dose. If you’re still in pain or get pain in between taking medicines, it’s important to tell your doctor or nurse.
Your doctor may also prescribe medicines for you to take if your pain gets worse or you get new symptoms like feeling sick. This means these medicines are available if you need them quickly or during the night. You might hear this called “anticipatory drugs”, “anticipatory prescribing” or “just in case medicines”.
If you find it hard to swallow tablets or liquids, your doctor or nurse can give you medicines in other ways, such as with a skin patch or an injection. They may also suggest using a syringe driver. A syringe driver is a small, battery-operated pump that will give you a continuous dose of pain-relieving medicine. Your medicines are put in a syringe, and the syringe driver pushes the medicines into your body through a needle, which is inserted under the skin on your arm, leg or tummy. Read more about ways to manage pain.
Sleeping and feeling drowsy
Most people will sleep for long periods of time when they are dying. Some people may feel drowsy when they’re awake and others may become completely unconscious. This may only last a few hours, or it may continue for days. Even if you aren’t able to respond to people around you, you may be able to hear them talking. It can be reassuring to hear people talking calmly to you or to have someone holding your hand.
Not recognising people
Some people become confused and don’t recognise the people around them. They might see or hear things that are not actually there. This can be caused by sleepiness, changes in the body or medicines. This can be upsetting. It can help if you and your loved ones know that this could happen. And it can help to be in a peaceful environment.
Feeling restless or agitated
Some men feel restless or agitated. These feelings can be caused by many things. They might be caused by worries about what is happening, or your surroundings. They can also be caused by physical problems such as difficulty emptying your bowels (constipation) or problems urinating.
Your doctor and nurse can look at things that could help. For example, they might make sure you are in a calm environment or answer any questions you have. They may give you medicines to help you feel less anxious or to manage physical problems.
Changes in skin temperature or colour
Some men’s hands and feet may feel cold for other people to touch. Their skin may become blotchy or blue. This can be caused by changes in their blood flow. It isn’t usually painful or uncomfortable.
Changes in breathing
Most men’s breath will become shallower and they might have longer pauses between breaths. This is because the body needs less oxygen.
There might also be a slight groaning or rattling noise when you breathe. Although this can sound distressing, it shouldn’t be uncomfortable. It might help for someone to change the position you’re in so that you’re lying on your side. And there are medicines that may help.
Loss of appetite
Some men don’t feel like eating or drinking. And in the final stages, you won’t need any food or drink.
If you’re not drinking, your mouth may feel dry. Getting someone to moisten your lips or mouth can make you feel more comfortable. Your doctor may also talk to you and your family about whether to use a drip to keep you hydrated.
Changes in urinating or bowel movements
Some men have fewer bowel movements and urinate less because they are eating and drinking less. Pain-relieving medicines can also cause constipation.
Tell your doctor or nurse if you feel constipated. They may be able to give you medicines to help empty your bowels and make you more comfortable. Or they might suggest that you drink more water or eat different food.
Some men lose control of their bladder or bowels. This is because the muscles in these areas relax. Nurses and other people looking after you can help to keep you clean and comfortable.
Feeling or being sick
Some men get nausea (feeling sick) or vomiting (being sick). This might be because of treatments, medicines or changes in your body. Your doctor or nurse may be able to give you medicines to help with the sickness. It is sometimes easier to have these medicines via an injection under the skin or via a syringe driver as it can be hard to swallow tablets when you feel sick.
Stopping medicines
Your doctor or nurse will review your medicines as you approach the end of your life. They will discuss with you if you wish to stop taking any medicines or look at other ways to give your medicines, such as injections or a syringe driver, if you have difficulty swallowing.
Getting more information about what to expect
- Download or order A guide for the end of life from Macmillan Cancer Support.
- Get more information on death and dying from Hospice UK and Sue Ryder.
- Find out more about homecare.
- Read more about End of life care on the NHS website.
- Find out about what happens after someone has died from Macmillan Cancer Support.
- Read more about other useful organisations.
References and reviewers
Updated: November 2023 | Due for Review: November 2024
- Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. Metastatic patterns of prostate cancer: An autopsy study of 1,589 patients. Hum Pathol. 2000 May;31(5):578–83.
- Caffo O, Gernone A, Ortega C, Sava T, Cartenì G, Facchini G, et al. Central nervous system metastases from castration-resistant prostate cancer in the docetaxel era. J Neurooncol. 2012 Mar 1;107(1):191–6.
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain (review). Cochrane Database Syst Rev [Internet]. 2013 [cited 2017 Feb 1];(10). Available from: http://doi.wiley.com/10.1002/14651858.CD010270.pub2
- Macmillan Cancer Support. The rich picture on people at end of life.
- Macmillan Cancer Support. The Rich Picture: People at the end of life. 2017.
- National Council for Palliative Care (NCPC). What to expect when someone important to you is dying: A guide for carers, families, and friends of dying people. 2015.
- National Institute for Clinical Excellence. NICE guideline 31: Care of dying adults in the last days of life [Internet]. NICE; 2015. Available from: http://www.nice.org.uk/guidance/ng31/resources/care-of-dying-adults-in-the-last-days-of-life-1837387324357
- National Institute for Health and Care Excellence. Palliative care for adults: strong opioids for pain relief. Clinical guideline 140. (modified August 2016); 2012.
- Salvati M, Frati A, Russo N, Brogna C, Piccirilli M, D’Andrea G, et al. Brain metastasis from prostate cancer. Report of 13 cases and critical analysis of the literature. J Exp Clin Cancer Res CR. 2005 Jun;24(2):203–7.
- Thompson JC, Wood J, Feuer D. Prostate cancer: palliative care and pain relief. Br Med Bull. 2007;83(1):341–54.
- Vinjamoori AH, Jagannathan JP, Shinagare AB, Taplin ME, Oh WK, Van den Abbeele AD, et al. Atypical Metastases From Prostate Cancer: 10-Year Experience at a Single Institution. Am J Roentgenol. 2012 Aug;199(2):367–72.
This information has been reviewed for accuracy and updated by:
- Our Health Information team
- Our Specialist Nurses.

